Full Text
History
The 1st question - Is it syncope?
The first step in the evaluation of syncope is to decide if the patient really has syncope or pre-syncope. Obtaining history from the patient is not always easy. Dizziness is so common a symptom that physician is sometimes unclear in which cases to investigate further or to refer to a cardiologist/Electro physiologist and when to just reassure the patient. Syncope that has led to injuries to the body should be taken very seriously however transient it may be. Sometimes patients who have syncope and suffer head injuries often have the injuries treated but evaluation of syncope is forgotten. Tonic clonic seizures usually indicate a neurological problem but one should remember that seizure like activity may also occur during cardiac arrest caused by ventricular fibrillation (VF) or with complete heart block. Many young children with congenital long QT syndrome and recurrent VF have been treated with multiple anti epileptic drugs with this mistaken diagnosis. Most often, the vital clues to diagnosis are obtained from history rather than from multiple tests. The sequence of events leading to syncope and the background medical history should dictate the investigations to be done in a particular patient. The person from whom the history is obtained is very important. Ideally if possible, history is best obtained from a witness to the syncope, as the recollection of events by the patient may be at variance with the true picture. The patient can however be relied upon to tell us the symptoms experienced prior to loss of consciousness, which can give a pointer to the diagnosis.
Different clinical situations
Vaso vagal or Neurocardiogenic syncope
By far this is the most common condition causing syncope. It can occur in any age group though more common in the elderly. Frequently encountered situations are when a child standing in the school for a long time, some individuals on seeing blood , hearing some unexpected news, extremes of emotions or smelling a noxious stimuli. Patients seek medical advice when they have recurrent symptoms. Typically these occur when the patient is in upright position often after sitting or lying down for a long time, like getting up in the middle of night to go to the toilet. They can occur during prolonged standing and infrequently in the sitting position too. They never occur in lying down position. The benign nature of these episodes is seen by the fact that patients experience these symptoms for many years before approaching a physician. After a few episodes some patients learn to recognize prodromal symptoms before syncope. The episodes are characteristically very transient half a minute to 2-3 minutes, and there are no sequelea following the episode. Syncopal episodes may however result in injuries. Tonic- clonic movements or seizures are not a part of this neither are bladder or bowel incontinence. If there is a trained observer, he may note that the pulse rate was low or weak at the time.
Sudden cardiac arrest
While neurocardiogenic syncope is most common, cardiac arrest is the most dangerous. In every patient with syncope this diagnosis must be deliberately considered and conclusively excluded. In fact the physician’s job is incomplete if he has not excluded this condition when dealing with a patient with syncope. What may be a self-terminating ventricular arrhythmia this time may result in sudden death next time. This condition should be suspected in any patient with syncope having history of myocardial infarction in the past, or ventricular dysfunction (Echocardiogram showing EF< 40%). This should also be considered in patients who have undergone coronary angioplasty or bypass surgery in the past or those with cardiomyopathies. It should be remembered that cardiac arrest could be the first manifestation of coronary artery disease (CAD) and patients with coronary risk factors having syncope should be actively investigated for the presence of CAD. Presence of chest pain preceding the syncope may point to the diagnosis but is not always present. Syncope in this situation is not posture related, but can get precipitated on exertion. It is transient and may be associated with severe sweating. The patient needs to be hospitalized for evaluation as these patients are at high risk of sudden death. Family history of sudden death should make one suspect inheritable genetic syndromes like long QT syndrome, or Brugada syndrome.
Arrhythmias and Conduction system disease
Apart from dangerous arrhythmias like ventricular tachycardia and fibrillation which can cause sudden cardiac arrest, other apparently benign arrhythmias like supraventricular tachycardia can also sometimes cause syncope when there are associated with very fast ventricular rates. Typically these patients experience palpitations first then lose consciousness if the tachycardia is too rapid compromising cardiac output. Once lying posture is achieved, blood pressure improves and they regain consciousness. This is also the mechanism in patients with paroxysmal atrial fibrillation (AF) who may experience syncope when the ventricular rates are very rapid. Syncope may also occur or when the fast AF suddenly terminates with a long pause, particularly with underlying sinus node disease. Ventricular tachycardia even when occurring in normal hearts can result in syncope. One of the causes of exertional syncope is RVOT VT .One of the eminently treatable causes of syncope is disease of the conduction system. Syncope occurs due to a long pause between ventricular complexes. Syncope is a very important symptom of advanced AV block and in this situation patient needs to be hospitalized. Sometimes these are transient and should be suspected in a patient with bradycardia or ECG showing LBBB or RBBB. Some of the drugs used in cardiovascular medicine may be responsible hence history of usage of medications like beta blockers, Digoxin, Amidarone must be carefully looked for. In a patient with suspected conduction disease occurrence of syncope on exertion may indicate an advanced AV block needing a pacemaker.
Neurological causes
Clinical picture that points to a neurological etiology includes associated seizures, focal neurological deficit, and presence of a carotid bruit. In the absence of these pointers, neurological work up is to be undertaken once common and life threatening cardiovascular causes are excluded. Every patient with syncope does not need CT/MRI of brain and conversely having a normal imaging of brain does not convey any conclusive information to the doctor.
Investigations
Every patient must have routine blood chemistry which includes complete blood picture, blood sugar, serum electrolytes, serum creatinine, and thyroid profile as a baseline. The most important factor influencing management of the patient is the presence of heart disease and hence ECG and echocardiogram constitute the front line investigations. Generally with few exceptions, if ECG and Echo are totally normal, life threatening causes of syncope can be excluded. It is important to remember that in a given patient all investigations need not be done. The clinical background and history should dictate the choice of tests to be done.
ECG/Holter
Many clues can be seen on ECG and in some cases the diagnosis is solely made with the help of ECG. Holter monitoring is an extension of ECG and is helpful in situations which are episodic. The presence of pathological Q waves indicates the presence of myocardial infarction of some duration, which would make the possibility of sudden cardiac arrest being responsible for syncope strong; the suspicion is increased if this is associated with frequent Ventricular ectopy. Reversible ST-T changes indicate presence of underlying ischemia. This and the presence of prolonged QT interval both make the occurrence of polymorphic VT possible which can lead to cardiac arrest. Prolonged QT may be acquired or may be present since birth in which situation it is termed as congenital long QT syndrome. Another condition increasing risk of cardiac arrest is the Brugada syndrome which is recognized in the ECG as presence of incomplete RBBB and ST elevation in leads V1 and V2. Sinus pauses or obvious AV block (more p waves than QRS complexes) suggest conduction system disease as cause of syncope and would need pacemaker implantation. The presence of sinus bradycardia alone may warrant electrophysiological studies to assess function of the sinus node.ECG showing RBBB or LBBB with or without prolonged PR interval (≥ 200 msec) should raise the suspicion of AV conduction block being responsible for syncope and these patients need to be further evaluated. Presence of LBBB and RBBB in the same individual at different time makes them at a high risk of complete heart block. Presence of increased QRS voltage in the precordial leads suggests ventricular hypertrophy and should be further investigated for Hypertrophic cardiomyopathy which is one of conditions that can lead to sudden death. Occurrence of ventricular ectopics of the same morphology consistently should make one consider the possibility of ventricular tachycardia. As arrhythmias occur episodically resting ECG may be normal in which case a holter or a long term rhythm monitoring device can document the arrhythmia when it occurs. Another important ECG finding is presence of pre excitation in a resting ECG, which is recognized by the presence of a short PR interval and a delta wave. These patients are prone to develop atrial fibrillation with fast ventricular rates which is manifested as a wide QRS irregular tachycardia that can lead to syncope.
Long term Rhythm monitoring
For patients whose syncope is infrequent, 24/48 hour holter is inadequate. Such patients need long term recording. One of them is implantable loop recorder which is implanted under the skin and can be kept in situ for few years. A noninvasive external recorder (ELR) is now made recently available which is wearable and can be used for a few months.
Echocardiogram
Echo clearly distinguishes patients who have structural heart disease from those who have not. By far this is the most cost effective investigation which helps in decision making in a patient with syncope and should be performed in all the patients. The most important information it gives is the assessment of ventricular function as a decreased ejection fraction makes the patient prone for cardiac arrest and sudden death. Presence of akinetic or dyskinetic segments or thinned out areas indicate scarring and fibrosis of the myocardium making it vulnerable for occurrence of VT /VF. Dilated left atrium or a LA thrombus should make one suspect paroxysmal atrial fibrillation. Dilated, restrictive or hypertrophic cardiomyopathies increase patients risk for malignant rhythms. Rarely cardiac tumors obstruct the valves compromising cardiac output and can lead to syncope.
Newer Imaging- Cardiac MRI
Assessment of structural abnormalities of heart has extended today beyond echocardiogram. Cardiac MRI is very useful in demonstrating ventricular myocardial scars and is a useful investigation in patients in whom cardiac arrest is suspected a cause for syncope. This is used today in patients with ischemic cardiomyopathies to demonstrate ventricular aneurysms or scars.
Treadmill test
Some patients have syncope on effort. This occurs in patients with some types of VT (RVOT VT) or advanced AV block. In such cases treadmill test may help to diagnose the cause of syncope. It is important to make sure that the ECG and Echo are normal before subjecting the patient to TMT. This is because severe aortic stenosis may cause exercise induced syncope but should not be subjected to this test. Patients with severe coronary artery disease may also experience syncope on effort.
Tilt table test
This is one of the underutilized and inexpensive tests largely because of unavailability in many hospitals. This test requires a tilt table which is usually a modified x ray table. It should be able to be tilted to 75 degrees and rapidly brought down to horizontal position if need arises. It is useful for the diagnosis of neurocardiogenic syncope. The advantages of this test are firstly as it reproduces the symptoms, the patients confidence is gained, the patient knows what causes his problem and what relieves it. Though not curable the diagnosis of Neurocardiogenic syncope clearly demonstrates the benign nature of the problem, and once positive obviates the need for further often expensive diagnostic testing. This test is ordered in a patient who has syncope on upright posture and whose echo and ECG are normal. There are 3 types of positive tilt test vasodepressor – associated with fall in blood pressure, Cardio inhibitory- associated with bradycardia and Mixed which has both drop in blood pressure and heart rates.
Electrophysiological study
In selected patients EP study can demonstrate the cause for syncope. The most important use of EP study is to identify patients having high risk of sudden death. EP study is indicated in patients with myocardial infarction in past, or having LV dysfunction presenting with syncope or dizziness. Ability to induce Ventricular tachycardia (VT) during EP study makes these patients at a high risk of sudden death and warrants implantation of ICD. Patients presenting with pre-syncope or syncope where the ECG shows a bifascicular block (RBBB with axis deviation, or LBBB) with or without prolonged PR interval, may undergo EP study. Demonstration of an infra hisian conduction disease in these patients by a prolonged HV interval or a H-V block, stratifies them as having a high risk for complete heart block in the future. One can assess sinus node function or hypersensitivity of carotid sinus .EP studies can also be used to induce suspected arrhythmias and these can be ablated offering a permanent cure for the patient’s problem. Radiofrequency ablation generally can be offered to patients with arrhythmias and structurally normal hearts. These are supraventricular tachycardia (SVT), WPW syndrome, RVOT VT, Fascicular VT, Atrial flutter, and atrial fibrillation.
Treatment: Following is a summary of various conditions that can present with syncope and their treatment options.
|
Diagnosis
|
Treatment
|
|
AV conduction disease
|
Pacemaker
|
|
Neurocardiogenic syncope
|
Medical, rarely pacemaker
|
|
SVT & WPW syndrome
|
Radiofrequency ablation
|
|
Ventricular tachycardia with normal Heart
|
Radiofrequency ablation
|
|
Spontaneous or inducible Ventricular tachycardia with LV dysfunction/ past MI/ Structural heart disease
|
ICD
|
|
Long QT syndrome
|
Beta blockers/ ICD
|
|
Hypertrophic cardiomyopathy/ Brugada syndrome
|
ICD
|
Following are some real life examples of patients presenting with syncope
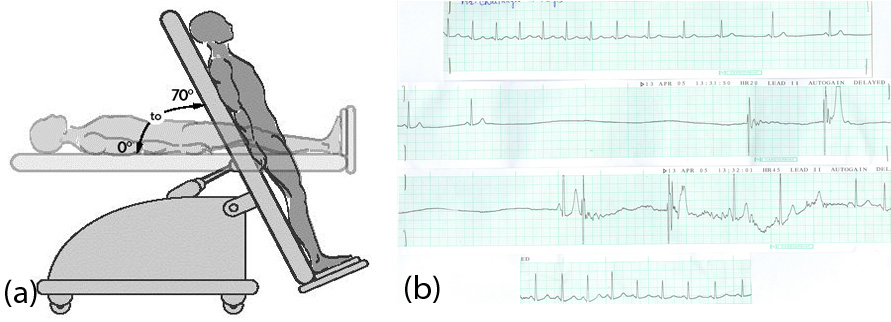
Figure 1: (A) Tilt table test used for diagnosis of vasovagal/neurocardiogenic syncope. (B) ECG in a patient undergoing tilt test showing a long pause. This was associated with significant drop in his blood pressure with syncope proving the diagnosis.
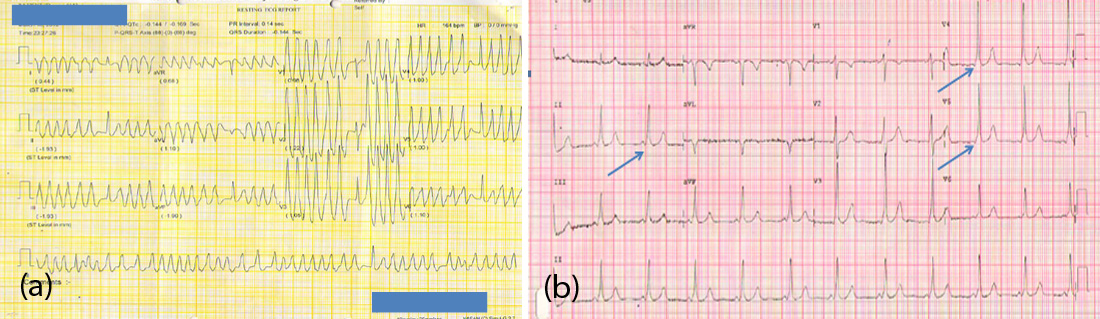
Figure 2: (A) Patient who presented with syncope was found to have wide QRS irregular tachycardia indicating atrial fibrillation with pre excitation. (B) He was cardioverted and ECG in sinus rhythm shows short PR interval and delta waves, showing that he had WPW syndrome. He underwent radiofrequency ablation curing him permanently.
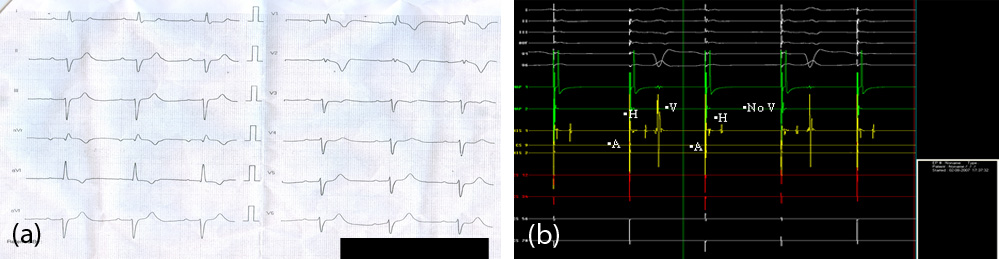
Figure 3: (A) 55 yr old lady with dizziness. ECG shows RBBB with left axis with prolonged PR interval. (B) EP study of this patient shows 2:1 AV block with atrial pacing at 100/minute. HIS channel shows infra hisian block. This indicates high degree AV block and a need for permanent pacemaker.
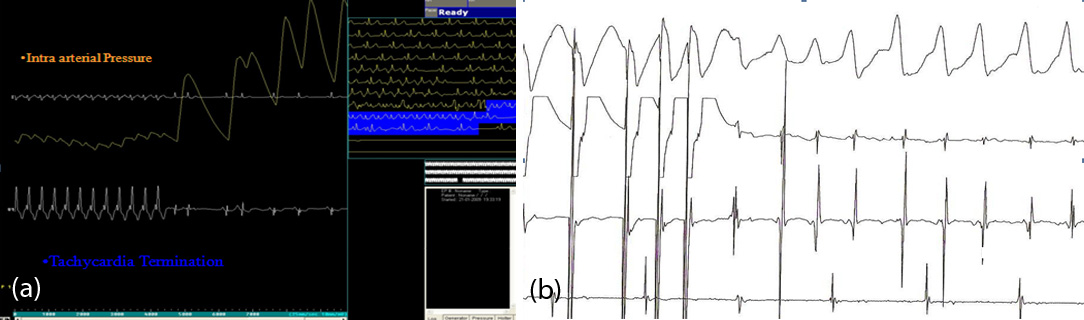
Figure 4: (A) EP study in a young lady with syncope. Induction of SVT is associated with a drop in blood pressure which recovers immediately with termination. The cause for syncope is established. She underwent a curative radiofrequency ablation. (B) EP study in a 50 year old man with MI 5 years back presenting now with syncope. On ventricular pacing VT is induced easily with drop in blood pressure. The study shows that he is at a high risk of sudden death. He was implanted an ICD.