Full Text
Introduction
The face is unique and the most crucial part of our identity. In plastic surgery, the function of the face is to look like the face. In other words, the facial 'form' is just as important as the function [1]. The face is divided into different regional units, all of which are adjacent and contiguous. This division is based on specific characteristics like skin quality, outline, and contour. Skin quality depends on the texture, colour, and hair-bearing attributes of the skin. Uniformity of skin colour and texture is the most crucial element of facial reconstruction, to restore a normal appearance. Other characteristics, like contour and outline, are also important. Reconstructive options for facial defects include healing by secondary intention, primary closure, split-thickness skin grafts, full-thickness skin grafts, local flaps, local flaps with tissue expansion, loco-regional flaps, and distant free-tissue microvascular flaps [2].
Ideally, an excellent reconstruction would replace the defect with similar kind of tissues, while being easy to perform. With increasing awareness of aesthetic outcomes, patients now expect more natural-looking results with lesser scars, especially over the face [3]. Skin grafts are easy to perform, but they produce a patchy appearance owing to their unpredictable colour and shiny texture, which does not match the surrounding normal facial skin. Even combinations of flaps and grafts do not have a satisfactory aesthetic outcome [4]. Considering all these factors, an enlarged and extended version of the classical cheek flap with well-camouflaged incisions provides excellent results in facial reconstruction [5]. Further extending the incision lines of extended facelift surgery in the posterior retroauricular and upper cervical regions would enable simultaneous flap dissection, advancement and rotation to adequately cover posttraumatic facial defects in adults. Deep-plane facelift-like dissection would ensure thicker flap with better vascularity to flap-tip for ample reconstruction of significant defects while minimising flap-loss. Amalgamating larger and thicker flaps based on these principles of an extended deep-plane facelift was termed ‘augmented facelift flap’.
Materials and methods
Medical records were retrospectively analysed between January 2009 and December 2019 for adult patients presenting with posttraumatic facial defects. Ten such patients who underwent primary facial reconstruction with an augmented facelift flap, and followed-up for at least six months postoperatively, were included. The study was conducted under the guiding principles of the Declaration of Helsinki. This study did not require IRB approval as both extended facelift and cheek flaps are established procedures. All patients were elaborated preoperatively about necessary surgeries, anaesthesia, intraoperative video recording, and photography. Consent was obtained after fully satisfying all their queries.
The patients’ age ranged between 21 and 78 years, with a mean of 49.3 years. The male to female ratio was 8:2. Six patients presented after automobile accidents, two after industrial workplace accidents, and two after falling from height or stairs. Six patients had defects over the medial cheek, two over the upper lateral cheek near the lateral orbital area, and two had defects over the lower eyelid along with medial cheek. The size of the defects ranged from 10.5 to 27 cm2. Patients with suspected defects to the brain and facial skeleton were assessed preoperatively by computed tomograms. Broad-spectrum antibiotics were started preoperatively in all patients and continued postoperatively.
Surgical technique
An augmented facelift flap design
Augmented facelift flap incorporated more tissues from adjacent facial areas like posterior retroauricular and upper cervical regions. Compared to traditional cheek flaps, it was larger, with a broader base and greater arc of rotation (Figure 1a). The flap marking started from the medial cheek or lower eyelid area medially and proceeded up to the lateral edge of the lower eyelid. It went across with a gentle arc through the sideburn hairs towards the helical root. Next, it descended as a curved incision along the anterior border of the helix until the tragus. It continued intra-tragal along the posterior border of the tragus, between the ear and the face. Then it extended along the sulcus between the earlobe and cheek and curved below the earlobe into the retroauricular region. It continued as a low retroauricular incision preserving the occipital hairline (Figure 1b). For reconstructing bigger defects, where more tissue recruitment was necessary, the incision line swept forward into the upper neck, along the lateral part of upper cervical crease (Figures 2c, 3b). Incisions in this flap design were based on extended facelift surgery, with medial and lateral extensions as required [6, 7].
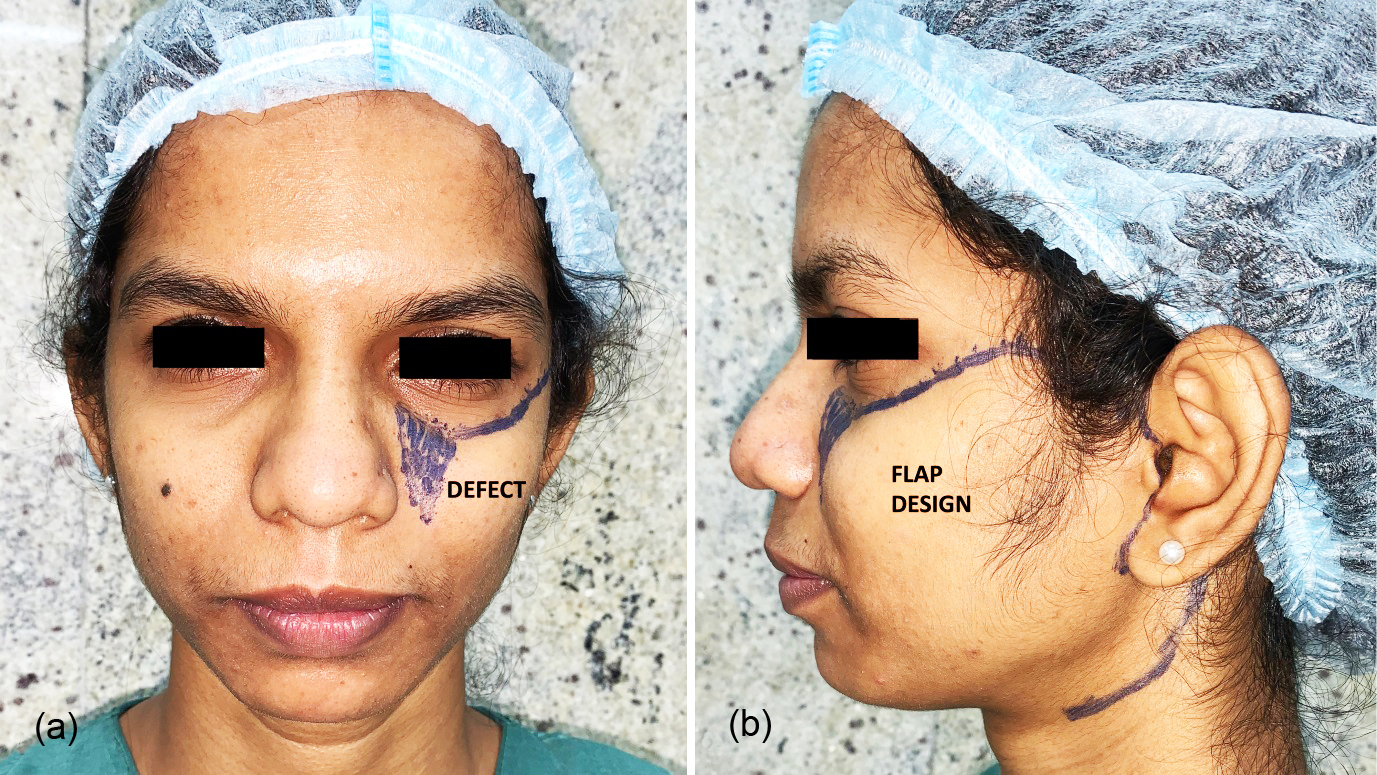
Figure 1: (a) Template of an upper-medial defect on a model face, marked in violet. (b) The markings of an augmented facelift flap design for reconstructing this defect.
An augmented facelift flap dissection
A tumescent solution (containing lidocaine 2%, bupivacaine 0.5%, normal saline and epinephrine 1:100,000) was infiltrated along the planes of dissection. For smaller defects and in patients where problems were deemed to be less likely, infiltration and flap elevation occurred in the subcutaneous tissue plane superficial to the SMAS (Figure 2c). Deep-plane dissection, wide elevation, and flap undermining deep to the superficial musculoaponeurotic system (SMAS) were performed for more extensive defects, where higher tension along the flap margins was more likely. Subcutaneous skin-flap dissection started over the pre-auricular area and continued into the malar region, undermining the skin until the lateral two-thirds of the zygomatic eminence (Figure 3c). Sub-SMAS dissection was performed laterally in the cheek through a vertical pre-auricular incision, freeing the SMAS from the underlying parotid fascia. Superiorly, it proceeded horizontally 1 cm below the zygomatic arch to preserve the frontal branch of the facial nerve, continuing up to the junction of the zygomatic arch with the body. Here, the incision angled superiorly over the malar eminence towards the lateral canthus for about 3-4 cm. Near the lateral orbital region, the incision proceeded inferiorly at a 90-degree angle towards the superior aspect of the nasolabial fold. Diligent division of the zygomatic retaining ligaments ensured proper flap mobilisation, thereby reducing tension to the edges. Malar sub-SMAS dissection was performed in the plane between the surface of lip elevators and the overlying subcutaneous fat with sharp curved scissors directed upwards. Meticulous dissection ensured that the surgical plane remained superficial to the facial mimetic muscles and prevented any underlying facial nerve injury (Figure 3d). Thus, flap dissection following the foot-steps of extended SMAS dissection in deep-plane facelifts ensured better vascularity to the flap-tip and minimised flap-loss while covering significant facial defects satisfactorily [8, 9]. A small suction drain was always placed at the base of the flap for at least two days.
Anchoring ‘key sutures'
Anchoring and resuspending the flap were crucial elements for obtaining a proper closure. The first key sutures were placed below the ear lobule, to secure the significant rotation obtained with this flap. The second key sutures anchored the flap laterally to the lower part of the temporal fascia. The third key sutures firmly anchored the flap to the periosteum over the lateral orbital rim. The fourth key sutures fixed the flap to the arcus marginalis, where the inferior orbital septum fused with the periosteum. These four sets of sutures prevented the pulling-down of the lower eyelid by the weight of the flap [10]. These precautions were essential to minimise lower-lid ectropion, flap ptosis, and upper lip imbalance, which are well-known complications of cheek flaps and its many modifications [11].
Results
Primary reconstruction achieved adequate soft-tissue coverage over the cheek, lateral orbit, and lower eyelid defects while matching the colour and texture satisfactorily. In one patient with a total lower eyelid defect, palmaris longus tendon graft was used to support the eyelid and buccal mucosal graft to reconstruct the posterior lamella of the eyelid. Complete or partial flap loss and infection were absent. Flaps were completely viable and healed well in eight patients (80%). Superficial necrosis of the upper dermo-epidermal layers of the skin occurred in one patient (10%), and it healed well over the next few months without any further intervention. Lower-lid ectropion with deep marginal necrosis for some length occurred in one patient (10%), and it healed with an indented scar. Venous stasis with bluish discolouration of the tip of the flap was seen in three patients (30%). Stasis settled down within a week or two without leaving any stigma.
A patient-reported outcomes questionnaire was used to measure overall patient satisfaction six months postoperatively. The questionnaire included (a) postoperative satisfaction with facial appearance, (b) improvements in quality of life, (c) ease of recovery and postoperative complications hampering daily life, and (d) overall satisfaction with the entire surgical process. All measurable points were tabulated on a visual analogue scale from 1-10, with 1 being the worst-imaginable and 10 being the best-imaginable outcome. An average of scores was tabulated in percentages. Patient-reported satisfaction scores ranged between 50% to 90%, with a mean of 78% (Table 1).
Table 1: The patient’s population.
|
ID
|
Age
|
Sex
|
Location
|
Aetiology
|
Size
|
Results/ Complications
|
Post-op VAS
|
|
1
|
68 y
|
M
|
Medial cheek
|
Automobile Accident
|
5×4.5 cm
|
Venous stasis at tip, healed well
|
70%
|
|
2
|
29 y
|
M
|
Upper cheek, lateral to eyes
|
Fall from height
|
4×3 cm
|
Good, no complication
|
80%
|
|
3
|
35 y
|
M
|
Medial cheek
|
Automobile Accident
|
4.5×3 cm
|
Good, no complication
|
70%
|
|
4
|
42 y
|
M
|
Medial cheek
|
Automobile Accident
|
4.5×4 cm
|
Good, no complication
|
80%
|
|
5
|
21 y
|
F
|
Lower eyelid and medial cheek
|
Industrial accident
|
5×3 cm
|
Venous stasis, Superficial epidermolysis
|
80%
|
|
6
|
52 y
|
M
|
Medial cheek
|
Automobile Accident
|
5×2.5 cm
|
Good, no complication
|
90%
|
|
7
|
78 y
|
F
|
Medial cheek
|
Automobile Accident
|
4×3.5 cm
|
Good, no complication
|
90%
|
|
8
|
58 y
|
M
|
Lower eyelid and medial cheek
|
Fall from height
|
6×4.5 cm
|
Deep marginal necrosis at edges
|
50%
|
|
9
|
49 y
|
M
|
Medial cheek
|
Industrial Accident
|
3.5×3 cm
|
Good, no complication
|
80%
|
|
10
|
61 y
|
M
|
Upper cheek, lateral to eyes
|
Automobile Accident
|
4×3.5 cm
|
Venous stasis at temple, healed well
|
90%
|
Sample case reports
Three cases are highlighted to demonstrate the reconstruction of cheek and eyelid defects with a facelift approach and augmented facelift flap.
Case 1 (Case ID 2)
A 29-year-old male patient presented to the emergency after a fall from a height, with necrosed skin and 4×3 cm sized injury over the forehead and cheek. The patient was counselled about different reconstructive options, including skin grafts and flaps. After considering all options, a decision to utilise a large flap was made because of the benefits listed below: (a) tension-less flap advancement would maximise vascularity and minimise necrosis at the tip and edges of the flap, (b) matching contour and colour from surrounding skin would ensure ‘like-for-like’, (c) fine suturing over tension-free flap margins would minimise scar problems later, (d) hiding most of the incisions within the natural facial lines and creases would make even a large flap imperceptible.
An augmented facelift flap was performed, incorporating excess skin from the retroauricular area and lateral neck. Incisional scars were camouflaged well. The patient had a near-normal appearance as early as two weeks postoperatively. Scars faded away over the next six months.

Figure 2: A 29-year-old man with defects over the lateral orbital area and forehead indicated with black arrows. (a) Frontal view, (b) Right oblique view, (c) Intraoperative photograph of augmented facelift flap showing the dissection of flap superficial to the subcutaneous musculoaponeurotic system, (d) Rotation-advancement of the flap to cover the facial wound, (e) Frontal view and (f) Right oblique view of the postoperative result after six months.
Case 2 (Case ID 5)
A 21-year-old female patient presented after an industrial accident with a 5x3 cm wound over the lower eyelid and medial cheek, near the nose-cheek junction. During extensive pre-operative counselling, this patient was offered multiple reconstructive options, including smaller rotation-advancement flaps and skin grafts. After seeing different results of facial reconstructions, the patient opted for an extensive flap reconstruction to ensure better survivability of the flap-tip, which was singularly crucial for successful results. An augmented facelift flap was dissected to advance and cover the defect. The flap extended along the subciliary margins superiorly until it reached the defect. The flap was extended to incorporate retro-auricular tissues. Mild venous stasis was seen at the tip of the flap during the initial postoperative period. Superficial epidermolysis developed after two weeks even as venous stasis settled by this time. Lower-lid ectropion with 2 mm of inferior scleral show was evident during the early postoperative period. Discolouration and ectropion improved steadily over the next six months with conservative measures like scar massage and cream application. Discolouration and ectropion were not discernible six months postoperatively. Long-term results were satisfying, and the patient went on to lead an active working life.

Figure 3: A 21-year-old lady presented with (a) a 5 x 3 cm wound over the lower eyelid extending to the medial cheek, (b) Augmented facelift flap was elevated, rotated, and advanced to cover the injury, (c) Coverage of the wound after flap inset. Venous stasis of the tip of the flap was evident in the immediate postoperative period, as indicated by a black arrow, (d) The rest of the flap margins remained healthy 48 hours postoperatively, during drain removal, (e) Superficial epidermolysis was present at the tip of the flap, indicated by a black arrow. Mild oedema of the subciliary margins and above the scar was visible. Lower-lid ectropion with 2 mm of inferior scleral show was apparent. (f) Flap healed well six months postoperatively. Lower-lid ectropion reduced within this period and the scleral show was negligible in the long-term. Discolouration and oedema resolved with conservative measures like scar massage and cream application, leading to a satisfying outcome.
Case 3 (Case ID 10)
A 61-year-old male patient presented to the hospital emergency after an automobile accident with multiple deep dirty wounds over his face. A 4×3.5 cm dirty wound was present in the upper cheek and lateral orbital region, with a second dirty wound over the right temple area. Adequate wound debridement followed by an augmented facelift flap was performed to cover both the defects primarily. Simultaneous facelift on the opposite side achieved facial symmetry and restored facial harmony. After achieving balance and harmony in his facial appearance, the patient expressed deep satisfaction with the final long-term results.

Figure 4: (a) Frontal view of a 61-year-old man presenting after an automobile accident, (b) Two dirty defects, marked by black arrows, were found over the lateral orbital region and the temple, (c) Augmented facelift flap raised and retracted, (d) A facelift performed on the opposite side. In c & d, white arrows indicate underlying facial tissues, and blue arrows indicate overlying SMAS and subcutaneous tissues. (e) Frontal view and (f) worm’s eye view of postoperative results after facial reconstruction on the right and matching facelift on the left side of the face.
Discussion
Reconstruction of cheek and lower eyelid defects with cheek flaps, cervicofacial flaps, or cervico-deltopectoral flaps are commonly performed because they provide an excellent match of skin quality, including colour and texture. Beare first described a facial flap in 1969 for reconstruction after orbital exenteration [12]. Mustarde described a skin-only rotation-advancement cheek flap in 1970, which was rapidly adopted by many surgeons worldwide [13]. It was mainly a random-pattern flap, with potential complications of flap-tip necrosis, lower eyelid ectropion, and imbalance of the upper lip [14]. The risk of tip necrosis is more in smokers and post-radiotherapy patients. Multiple studies have shown that this disadvantage is avoided by deep-plane dissection, underneath the SMAS [15].
Lower-lid ectropion is another known complication of cheek and cervicofacial flap designs. The sheer weight of a large and heavy flap pulls down the thin periorbital skin and lower eyelid, distorting eyelid anatomy. Subcutaneous dissection between the skin and SMAS usually avoids these problems, but chances of tip necrosis are higher when superficial flaps are elevated to cover significant defects [16]. Flaps raised at a deep-plane and undermined widely are safer, with better vascularity to the flap-tip. However, they are more cumbersome and more prone to cause ectropion [17]. Eyelid tightening procedures are required to limit the extent of ectropion, either primarily or secondarily [18].
Classic cheek flap was modified several times by different surgeons. In one of these modifications, Schrudde described an angle-rotation flap, which extended the flap design behind the ear at a sixty-to-ninety-degree angle, mobilising retroauricular tissues for better coverage [19]. For coverage of more medially located defects, modifying this flap design by extending incision from retroauricular to upper cervical tissues with a curved incision (as a back-cut), rectified this problem [20]. In this series, incision lines followed that for extended facelift surgery, with low retroauricular extension and incorporating lateral upper neck tissues if necessary (Figures 1b, 2c & 3d).
Earlier, significant-sized flaps combining forehead and scalp tissues were performed for reconstructing large forehead defects. Effective reconstruction with minimal complications and good patient-reported outcomes were observed [21]. A similar approach over the face necessitated raising large and thick facial flaps even for smaller defects. A large flap minimises tension, flap-edge necrosis, and scar stretching; resulting in more acceptable long-term outcomes [22]. Facial flaps raised superficial to the SMAS to cover smaller defects are easy to dissect and does not consume excessive operative time. For significant facial defects, however, extensively dissecting deep-plane facelift-like flaps requires specialised knowledge of the facial anatomy, a steep learning curve, and entails more operative time and effort. This extra effort is vindicated after obtaining satisfying long-term results with minimal complications in a vast majority of patients. Consequently, an augmented facelift flap becomes a worthwhile option for reconstructing facial defects to both the patients and plastic surgeons.
Conclusion
An augmented facelift flap successfully reconstructs posttraumatic facial defects over the cheek, lateral orbit, and lower eyelids. This flap design enables the surgeon to infiltrate, dissect, elevate, and rotate the flap simultaneously for better mobilisation, thus providing excellent control over the extent of incision and dissection. It is relatively safe with fewer complications. Overall postoperative results are satisfactory with pleasing aesthesis and high patient acceptance rates. Thus, better aesthetic and functional outcomes are achieved by applying the principles of extended and deep-plane facelift surgery to facial reconstruction.
Consent
Patients were preoperatively informed through elaborate written consent about all surgical procedures, anaesthesia, intraoperative video recording, and photography.
Acknowledgement
I am grateful to Sister Swarnapriya Das for volunteering to be a model for the augmented facelift flap design, and to Mr. Goutam Bhowmick for his help in obtaining patient details.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Zide BM. Grabb and Smith's plastic surgery. Cheek reconstruction. Philadelphia: Lippincott-Raven; 1997.
[2] Mathes SJ, Nahai F. Clinical applications for muscle and musculocutaneous flaps. St Louis, MO. CV Mosby. Second Edition. 2010; pp.739.
[3] Rapstine ED, Knaus WJ, Thornton JF. Simplifying cheek reconstruction: A review of over 400 cases. Plast Reconstr Surg. 2012; 129(6):1291–1299.
[4] Roth DA, Longakel MT, Zide BM. Cheek surface reconstruction: best choices according to zones. Operat Tech Plast Reconstr Surg. 1998; 5(1):26–36.
[5] Heller L, Cole P, Kaufman Y. Cheek reconstruction: Current concepts in managing facial soft tissue loss. Semin Plast Surg. 2008; 22(4):294–305.
[6] Stuzin JM, Baker TJ, Gordon HL, Baker TM. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg. 1995; 22(2):295–311.
[7] Stuzin JM. Aging face and neck. In: Mathes SJ, editor. Plastic surgery. Philadelphia: Saunders Elsevier; 2006.
[8] Stuzin JM, Baker TJ, Gordon HL. The relationship of the superficial and deep facial fascias: relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992; 89(3):441–449.
[9] Mendelson BC. Extended sub-SMAS dissection and cheek elevation. Clin Plast Surg. 1995; 22(2):325–339.
[10] Harris GJ, Perez N. Anchored flaps in post-Mohs reconstruction of the lower eyelid, cheek, and lateral canthus: avoiding eyelid distortion. Ophthalmic Plast Reconstr Surg. 2003; 19(1):5–13.
[11] Boutros S, Zide B. Cheek and eyelid reconstruction: The resurrection of the angle rotation flap. Plast Reconstruct Surg. 2005; 116(5):1425–1430.
[12] Beare R. Flap repair following exenteration of the orbit. Proc R Soc Med. 1969; 62 (11 Part 1):1087–1090.
[13] Mustardé JC. The use of flaps in the orbital region. Plast Reconstr Surg. 1970; 45(2):146–150.
[14] Mustarde JC, Whitaker L. Repair and reconstruction in the orbital region. A practical guide. Plast Reconstr Surg. 1981; 67(5):692.
[15] Jacono AA, Rousso JJ, Lavin TJ. Comparing rates of distal edge necrosis in deep-plane vs. subcutaneous cervicofacial rotation-advancement flaps for facial cutaneous Mohs defects. JAMA Facial Plast Surg. 2014; 16(1):31–35.
[16] Austen WG, Parrett BM, Taghinia A, Wolfort SF, Upton J. The subcutaneous cervicofacial flap revisited. Ann Plast Surg. 2009; 62(2):149–153.
[17] Tan ST, MacKinnon CA. Deep plane cervicofacial flap: A useful and versatile technique in head and neck surgery. Head & Neck. 2006; 28(1):46–55.
[18] Becker FF, Langford FPJ. Deep-plane cervicofacial flap for reconstruction of large cheek defects. Arch Otolaryngol Head Neck Surg. 1996; 122(9):997–999.
[19] Schrudde J, Beinhoff U. Reconstruction of the face by means of the angle-rotation flap. Aesthetic Plast Surg. 1987; 11(1):15–22.
[20] Al Shetawi AH, Quimby A, Fernandes R. The cervicofacial flap in cheek reconstruction: a guide for flap design. J Oral Maxillofac Surg. 2017; 75(12):2708.e1–2708.e6.
[21] Saha S. Triple-plane dissection of combined forehead and scalp flaps for large posttraumatic forehead defects. Int J Recent Surg Med Sci. 2020; 6(01):24–29.
[22] Cole EL, Sanchez ER, Ortiz DA, Maguire PD. Expanded indications for the deep plane cervicofacial flap: Aesthetic reconstruction of large combined temporofrontal and brow defects. Ann Plast Surg. 2015; 74(5):543–548.