Case Report
2018
March
Volume : 6
Issue : 1
Imaging of vesicovaginal fistula using volume rendering technique by 16-Slice multidetector CT
Sumana B, Sahaja K, Swaroopa K, Kalyani B, Bhanu Murthy, Rao VRK
Pdf Page Numbers :- 28-31
Sumana B1,*, Sahaja K1, Swaroopa K1, Kalyani B1, Bhanu Murthy2 and Rao VRK1
1Department of Radiology, Great Eastern Medical School & Hospital, Ragolu, Srikakulam 532 484, Andhra Pradesh, India
2Department of Urology, Great Eastern Medical School & Hospital, Ragolu, Srikakulam 532 484, Andhra Pradesh, India
*Corresponding author: Sumana B, Department of Radiology, Great Eastern Medical School & Hospitals, Ragolu, Srikakulam, Andhra Pradesh- 532 484, India. Email: sumana.roses7@gmail.com
Received 19 September 2017; Revised 14 November 2017; Accepted 29 November 2017; Published 12 December 2017
Citation: Sumana B, Sahaja K, Swaroopa K, Kalyani B, Murthy B, Rao VRK. Imaging of vesicovaginal fistula using volume rendering technique by 16-Slice multidetector CT. J Med Sci Res. 2018; 6(1):28-31. DOI: http://dx.doi.org/10.17727/JMSR.2018/6-5
Copyright: © 2018 Sumana B et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Vesicovaginal fistula (VVF) is a communication between the posterior wall of urinary bladder and the vagina. VVF occurs most frequently, post hysterectomy, during obstructed labour and post radiation mainly for carcinoma cervix. Computed tomographic (CT) cystography has the distinct advantage of precisely demonstrating the communication between urinary bladder and the genital tract. For a successful repair and prevention of recurrence accurate diagnostic evaluation and timely repair with interposition flaps is mandatory.
Keywords: vesicovaginal fistula; urinary incontinence; hysterectomy; radiation
Full Text
Introduction
Vesicovaginal fistula (VVF) is one of the most common urogenital fistulous tracts with a communication between the posterior wall of urinary bladder and the vagina. It is mostly seen in the developing countries and rarely in the developed countries. Its incidence is 3 in 1,00,000 in West Africa alone. The most common causes that lead to its formation include gynecological procedures like hysterectomy, prolonged labor where there is pressure necrosis of bladder due to impaction between fetal head and pubic bone [1, 2]. Radiological imaging has a significant role in diagnosis and management of genitourinary tract injuries. Retrograde urethrography, voiding cystourethrography, intravenous urography and scintigraphy have been routinely used to investigate these patients. In recent times, multidetector CT (MDCT) scanner and MRI scanning are more effectively utilized for precise localization of the communication. Investigations such as cystoscopy, CT and MRI accurately define the fistulous tract. Advanced MRI sequences using three-dimensional Half-Fourier MRI acquisition and T2-weighted sequences with fat saturation are designed to visualize fluid filled spaces or tracts with precision without use of contrast media. We report two patients having post-hysterectomy VVF investigated by CT cystography and intravenous contrast enhanced delayed examination.
Case report
Case 1
A 40-year-old female operated for hysterectomy one month ago presented with dribbling of urine through vagina and urethral orifices associated with stress incontinence. Cystoscopy was performed under local anaesthesia which showed a defect of 2 cm in supratrigonal region. Both ureteral orifices were visualized separately. Urinary bladder was catheterized and 150 ml of dilute non-ionic contrast medium (Omnipaqe 350) was injected to distend the bladder. Radiography in lateral and oblique views showed simultaneous filling of the vagina but did not demonstrate the exactlocation of the fistulous tract (Figure 1). An immediate CT scan of pelvis was performed and the fistulous tract between the trigone of urinary bladder and the vaginal vault was confirmed both on sagittal and 3D reformatted images. Transabdominal fistulous repair of the tract and bivalving of the bladder were performed till the VVF opening. The fibrous tissue around the tract was removed along with the tract. An interpositional flap of greater omentum was placed 1-2 cm distal to the tract. Post-operative recovery was uneventful.
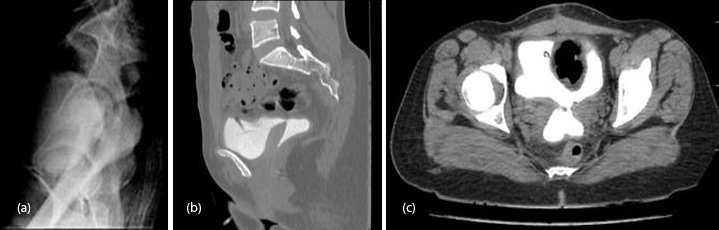
Figure 1: (a) Retrograde cystogram - Lateral view shows faint opacification of the cervix and vagina, the communication site or the tract are not demonstrable; (b, c) CT scan of Pelvis. Residual iodinated contrast following cystography is noted in the bladder and vagina. The communicating tract between the two is clearly shown consistent with a VVF.
Case 2
A 30-year-old female hysterectomized two months ago presented with urinary incontinence from two months and fever for five days. Cystoscopy showed focal defect in the posterior wall of urinary bladder communicating with the vaginal vault. Intravenous urography was performed by injecting 40 ml of Omnipaque contrast medium into the medial cubital vein and delayed computed tomography scan (CT) after 15 minutes was performed using MDCT scanner (16-Slice, General Electric) with 3D volume rendered reconstruction (kV 80, mA 150, matrix 512) and reconstruction slice thickness 0.625 mm. The contrast opacified oblong pear shaped cervical cavity was visualized posterior to the opacified urinary bladder. A small communicating tract at the dome of urinary bladder connecting to the vagina at a higher level was observed (Figure 2). Through transabdominal approach the fistulous tract was excised along with the fibrous tract around. Patient made uneventful post-operative recovery.
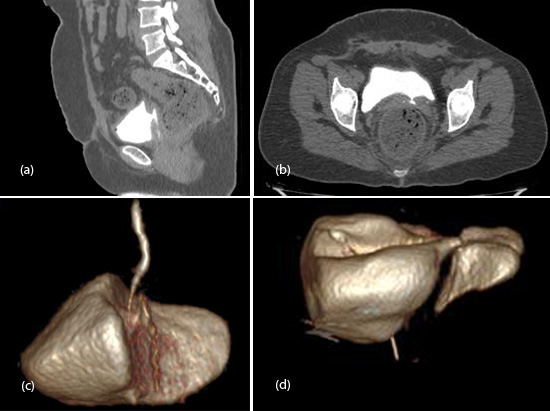
Figure 2: (a, b) CT scan of pelvis- Sagittal and axial sections demonstrate contrast filled urinary bladder with a communicating tract from the posterior wall to the vaginal vault, following intravenous injection; (c) 3D volume rendered image of urinarybladder revealsthe communicating tract clearly confirming the fistulous communication; (d) 3D volume rendered image of urinary bladder precisely reveals the communication with the vagina posteriorly.
Discussion
Ureterovaginal and VVF are the most common genito urinary fistulae. VVF may be congenital or acquired. There are two types of VVF, simple and complex. VVF occurs most frequently post hysterectomy, prolonged labor due to obstruction, post radiationmainly for carcinoma cervix and other pelvic malignancies such as bladder and endometrial carcinoma. The other conditions that lead to the formation of fistula are anterior colporrhaphy, cystocele repair and surgery for incontinence. According to Ibrahim et al. early marriage and child bearing, low literacy rate and poor antenatal care are the socio economic causes of obstetric fistulae formation [1]. Simple fistula measures greater than 0.5 mm without any complications whereas complex fistula measures less than 2.5 mm mostly due to previous fistulous repair. Symptoms such as urinary incontinence andinfection are most likely the presenting features of this condition. It also leads to continuous wetness, odor and discomfort to the patient. For a successful and timely repair it is very essential to know the exact location, size and number of fistulae. Methylene blue test can be performed to demonstrate the communication while a tampon is inserted into vagina, and the bladder is filled with the dye. Imaging modalities include retrograde urethrography, cystography, voiding cystourethrography, intravenous urography (IVU) and scintigraphy with Tc99m diethylenetriaminepentacetic acid helps in delineating the abnormality but do not provide necessary anatomical detail [3]. Conventional IVU and cystography often fail to show the anatomical details due to superimposing bony pelvic structures particularly in the lateral projection. MDCT using thin-section images (0.5 to 0.625 mm reconstruction increment) is a sensitive and specific modality for detection of these fistulae due to high spatial and temporal resolution [4, 5]. MDCT urography accurately reveals the fistula between the hollow organs. A vaginal tampon with MDCT cystography helps in delineating the VVF where the tampon acts as a negative contrast on pre contrast scan if there is no fistula [5, 6]. It behaves as a positive contrast in the presence of a VVF. Single-shot turbo spin echo using three-dimensional Half-Fourier MRI acquisition, T2-weighted sequences with fat saturation and long TR and long TE are used to visualize the entire urinary tract. Breath-hold acquisitions combined with thick slabs demonstrate the bladder in various projections. Submillimeter slices in 3D volume rendering and maximum intensity show the fistulous track in different planes. The sensitivities of conventional cystography, intravenous urography, CT urography and MRI were 40%, 0%, 50%, and 100%, respectively [7]. Small fistulae close spontaneously within two months of post ureteral catheterization and anti-cholinergic medications. Transvaginal approach is superior to transabdominal because of less complication, reduced hospital stay, less blood loss and less pain following the procedure. Ureteral occlusion and permanent nephrostomy are performedin patients who are unfit for surgery.
Conclusion
Conventional intra venous urography and cystography often fail to show the anatomical details due to superimposing bony pelvic structures. 3D CT scan volume rendered reconstruction is an excellent tool for effectively demonstrating the communication. Acknowledgement The Director, Great Eastern Medical School & Hospital, Srikakulam, India.
Conflictsof interest
The authors declare no conflicts of interest.
References
[1] Waaldijk K. Surgical classification of obstetric fistulas. Int J Gynecol Obstet. 1995; 49(2):161–163.
[2] Miller EA, Webster GD. Current management of vesicovaginal fistulae. Curr Opin Urol. 2001; 11(4):417–421.
[3] Botsikas D, Caviezel A, Becker CD. A new MDCT technique for the detection and anatomical exploration of urogenital fistulas. AJR Am J Roentgenol. 2012; 198(2):W160–W162.
[4] Avritscher R, Madoff DC, Ramirez PT, Wallace MJ, Ahrar K, et al. Fistulas of the lower urinary tract: Percutaneous approaches for the management of a difficult clinical entity. Radiographics. 2004; 24 Suppl 1:S217–236.
[5] Wah TM, Spencer JA. The role of CT in the management of adult urinary tract trauma. Clin Radiol. 2001; 56(4):268–277.
[6] Kawamoto S, Horton KM, Fishman EK. Computed tomography urography with 16-channel multidetector computed tomography: A pictorial review. J Comput Assist Tomogr. 2004; 28(5):581–587.
[7] Abou-El-Ghar ME, El-Assmy AM, Refaie HF, El-Diasty TA. Radiological diagnosis of vesicouterine fistula: Role of magnetic resonance imaging. J Magn Reson Imaging. 2012; 36(2):438–442.