Full Text
Introduction
Kegel first described the use of pelvic floor muscle (PFM) exercises to treat urinary incontinence in 1948 [1]. He reported a high success rate of 84% in his study. This early study did not differentiate between urge, stress, or other forms of incontinence. However, later studies have demonstrated that PFM exercises may be effective in treatment of symptoms of overactive bladder. The basis of such exercises is the observation that electrical stimulation of PFM appears to inhibit detrusor contractions. An early study by Godec [2] demonstrated decreased bladder hyperactivity and increase in bladder capacity after mild electrical stimulation, and deGroat [3] noted increased sympathetic firing during bladder filling, representing guarding reflexes to promote continence.
Anatomy
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling. Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed (Figure 1).
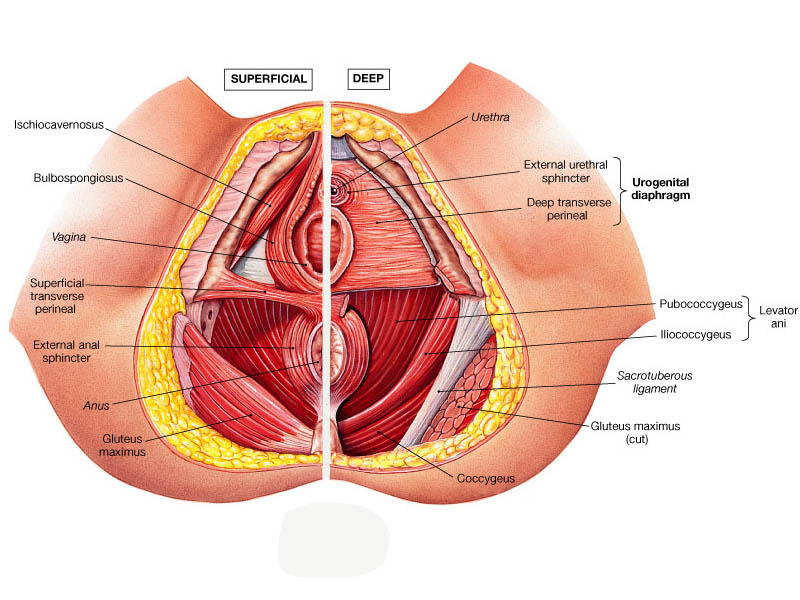 Figure 1: The most posterior part of the levator ani.
Figure 1: The most posterior part of the levator ani.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
Function
It is important in providing support for pelvic viscera (organs), e.g. the bladder, intestines, the uterus (in females), and in maintenance of continence as part of the urinary and anal sphincters.
Clinical significance
In women, the levator muscles or their supplying nerves can be damaged in pregnancy or childbirth, hysterectomy. Pelvic surgery using the "perineal approach" (between the anus and coccyx) is an established cause of damage to the pelvic floor. Damage to the pelvic floor not only contributes to urinary incontinence but can lead to pelvic organ prolapse. The vagina is suspended by attachments to the perineum, pelvic side wall and sacrum via attachments that include collagen, elastin, and smooth muscle. The pelvic floor muscles can be strengthened with Kegel exercises.
Pelvic floor exercise (PFE), also known as Kegel exercises, improve the tone and function of the pelvic floor muscles, which is of particular benefit for women who experience stress urinary incontinence. PFE generally is ineffective for urinary incontinence unless performed with biofeedback and trained supervision. Pelvic floor muscle tone may be estimated using a perineometer, which measures the pressure within the vagina.
How to do Kegel exercises
Identification of Kegel muscles requires proper training and improper exercises will not yield any benefits, Physiotherapist will guide you to identify the right muscles to strengthen to develop control. i) Find the right muscles: To identify your pelvic floor muscles, stop urination in midstream. If you succeed, you have identified the right muscles. ii) Perfect your technique: Once you have identified your pelvic floor muscles, empty your bladder and lie on your back. Tighten your pelvic floor muscles, hold the contraction for five seconds, and then relax for five seconds. Try it four or five times in a row. Work up to keeping the muscles contracted for 10 seconds at a time, relaxing for 10 seconds between contractions. iii) Maintain your focus: For best results, focus on tightening only your pelvic floor muscles. Be careful not to flex the muscles in your abdomen, thighs or buttocks. Avoid holding your breath. Instead, breathe freely during the exercises. iv) Repeat 3 times a day: Aim for at least three sets of 10 repetitions a day.
Review of literature
Nygaard et al. [4] recently reported use of pelvic floor exercises in the treatment of overactive bladder (OAB). They report a significant decrease in mean number of incontinent episodes per day in a group of 14 women studied over 3 months. Fifty percent of the patients described excellent or good results. It is important that the patient be properly educated regarding pelvic floor anatomy and assessed by a trained examiner for performance of exercises. The typical protocol calls for 50 contractions per day in two or three divided sessions. Each contraction is sustained for five seconds followed by 10 seconds of relaxation.
Conclusion
It is important to learn to do the exercises in the right way, and to check from time to time that you are still doing them correctly; biofeedback is added to aid in identification of appropriate muscle contractions. Multicomponent behavioral training, biofeedback and Kegel exercises are performed for the pelvic floor muscle training that increase urethral pressure to prevent urine loss.
Conflict of interest
The author declares no conflict of interest.
References
1. Kegel AH. Progressive resistance exercise in the functional restoration of the perineal muscles. Am J Obstet Gynecol. 1948; 56:238–248.
2. Godec C, Cass A, Ayala G. Bladder inhibition with functional electrical stimulation. Urology 1975; 6:663–666.
3. de Groat WC. A neurologic basis for the overactive bladder. Urology 1997; 50(6A Suppl):36–52.
4. Nygaard IE, Kreder KJ, Lepic MM, Fountain KA, Rhomberg AT. Efficacy of pelvic floor muscle exercises in woman with stress urge, and mixed urinary incontinence. Am J Obstet Gynecol. 1996; 174:120–125
5. Burgio KL, Locher JL, Goode PS. Combined behavioral and drug therapy of urge incontinence in older women. J Am Geriatr Soc. 2000; 48(4):370–374.
6. Das AK, White MD, Longhurst PA. Sacral nerve stimulation for the management of voiding dysfunction. Urology 2000; 2(1):43–52.
7. Dwyer PL, Lee ETC, Hay DM. Obesity and urinary incontinence in women. Br J Obstet Gynecol. 1988; 95:91–96.
8. Liberman JN, Hunt TL, Stewart WF, Wein A, Zhou Z, et al. Health-related quality of life among adults with symptoms of overactive bladder: results from a U.S. community-based survey. Urology 2001; 57(6):1044–1050.