Case Report
2017
March
Volume : 5
Issue : 1
Rare presentation of systemic lupus erythematosus
Deepti Sripurna, Sarath Chandra Mouli Veravalli, Prassana PV, Datta AS
Pdf Page Numbers :- 45-47
Deepti Sripurna1, Sarath Chandra Mouli Veravalli1, Prassana PV1,* and Datta AS1
1Department of Rheumatology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
*Corresponding author: Dr. Vijaya Prasanna, Department of Rheumatology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Email: prasanna.parimi.vijaya@gmail.com
Received 05 October 2016; Revised 17 November 2016; Accepted 22 December 2016; Published 30 December 2016
Citation: Sripurna D, Chandramouli VS, Prassana PV, Datta AS. Rare presentation of systemic lupus erythematosus. J Med Sci Res. 2017; 5(1):45-47. DOI: http://dx.doi.org/10.17727/JMSR.2017/5-9
Copyright: © 2017 Sripurna D, etublished by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Systemic lupus erythematosus is a prototype systemic autoimmune disease with varied presentations. Cutaneous and musculoskeletal manifestations are common clinical presentations. Severe disease activity results in multiorgan involvement among which kidneys are commonly affected in first two years after the onset of disease. Normally nonspecific cutaneous manifestations correlate with disease activity. Among such cutaneous manifestations Steven Johnsons and toxic epidermal necrolysis, which were associated with high mortality in lupus, were rarely reported. Periodic assessment of disease activity and severity are important to minimize high mortality and morbidity associated with this disease.
Keywords: toxic epidermal necrolysis; systemic lupus erythematosus
Full Text
Systemic lupus erythematosus (SLE) is a prototype autoimmune disease primarily affecting women of child bearing age. Cutaneous manifestations are one of the most commonly presenting features of lupus. They are classified as lupus specific and nonspecific lesions. Among them malar rash, discoid rash are commonly seen. In these patients, less common lesions like urticaria, bullous lesions often pose a diagnostic challenge when they are the sole presenting features. In this regard a rare presentation of lupus, as toxic epidermal necrolysis (TEN), is described here.
Case presentation
A 19-year-old girl presented with joint pains and constitutional symptoms for 5 months. Elsewhere she was started on disease-modifying antirheumatic drugs (DMARDs) and defaulted after one month. Gradually in the next five months she had worsening of constitutional symptoms. She presented to the emergency department with sudden onset of pain with redness of eyes and vesiculobullous rash involving mucosal sites, face, trunk and extremities (Figure 1).

Figure 1: Vesicobullar rash over back and chest.
There was no history of any drug intake in the last 4 months. There was photosensitivity and increased severity of joint pains. No history suggestive of Raynauds. On there is evidence of eyelid edema with erythema and crusting [1], vesiculobullous rash over trunk, extremities, orogenital regions, rash over face on clinical examination (Figure 2). Tachycardia and tachypnea and high blood pressure, were recorded.

Figure 2: (a) Crusting of eyelids with erythema, (b) Crusting of lips with oral ulcers.
Her serology revealed 3+, homogenous ANA and positive anti ds DNA and low complements. There was evidence of renal involvement in the form of new onset hypertension, subnephrotic range of proteinuria, elevated blood urea and serum creatinine. Her 2D Echo showed global hypokinesia with dilated left atrium (LA), severe left ventricle (LV) dysfunction, dilated, plethoric IVC. She also had serositis (pleural and pericardial). Her skin biopsy showed orthokeratosis of epidermis and transepidermal coagulative necrosis with exocytosis composed of lymphocytes, eosinophils and nuclear debris (Figure 3). Complete detachment of epidermis was seen. Dermis showed thin walled vessels with perivascular lymphoid infiltrate. Skin biopsy features were consistent with TEN.
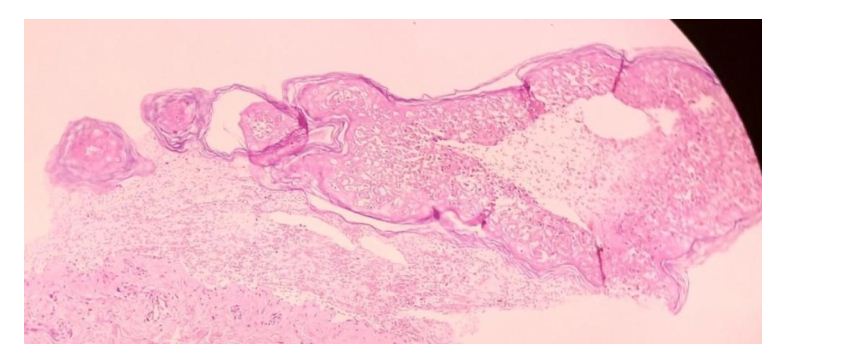
Figure 3: Skin biopsy consistent with features of TEN.
She was diagnosed as SLE with lupus nephritis, myocarditis, pseudomembranous conjunctivitis and cutaneous lesions as TEN which is a rare cutaneous manifestation presenting as the first manifestation of severe lupus in her [1].
She was given intravenous Immunoglobulin (IVIG) – 5gm/ day for 5 days, pulse steroids with which vesiculobullous rash improved. Symblepharon ring placement was done with amniotic membrane grafting [2].
She developed sudden onset of shortness of breath with falling saturations followed by bradycardia and expired. The probable reasons considered in view of this acute manifestations were alveolar haemorrhage, pulmonary edema, worsening myocarditis with failure, and pericardial tamponade.
Discussion
Cutaneous manifestations of lupus with or without musculoskeletal involvement is the common form of presentation. Among the nonspecific cutaneous features TEN is very rarely described in lupus. It is characterized by massive epidermal injury with severe alterations in dermoepidermal junction and subsequent apoptosis [3]. Underlying mechanism is thought to be due to exaggerated keratinocyte apoptosis because of increased Fas expression [4]. Drug induced TEN is more commonly seen than TEN as a disease manifestation in connective tissue disorders, as prolonged treatment with multiple drugs leads to TEN. These lesions cannot be differentiated from drug induced TEN though they occur predominantly in photodistribution areas. Subacute presentation is seen with painless oral ulcers. Positive ANA, dsDNA with low complements and haematological abnormalities and proteinuria, help in diagnosis [5].
TEN in lupus were classified by Sontheimer [6] into (a) TEN like acute cutaneous LE, (b) TEN like subacute cutaneous LE, (c) TEN in SLE not having LE specific lesions, (d) Vesiculobullous changes at active border of advancing annular subacute cutaneous LE, and (e) Vesiculobullous chronic cutaneous LE.
Conclusion
SLE is an autoimmune systemic disease involving multiple organs. If unchecked, mortality and morbidity are high. The rate of drug discontinuation is very high among patients, in view of chronicity of disease. Awareness about the disease and importance of drug compliance must be emphasized. The rare forms of common organ involvement can be the first presentation of the disease such as TEN like presentation as in this patient.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Sotozono C, Ueta M, Koizumi N, Inatomi T, Shirakata Y, et al. Diagnosis and treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis with ocular complications. Ophthalmology. 2009; 116(4):685–690.
[2] Zarbin M, Chu D, Liang L, Sheha H, Gregory DG, et al. Amniotic membrane transplantation as a new therapy for the acute ocular manifestations of Stevens-Johnson syndrome and toxic epidermal necrolysis. Surv Ophthalmol. 2009; 54(6):686–696.
[3] Maldelcorn R, Shear NH. Lupus-associated toxic epidermal necrolysis: A novel manifestation of lupus? J Am Acad Dermatol. 2003; 48(4):525–529.
[4] Abe R, Shimizu T, Shibaki A, Nakamura H, Watanabe H, et al. Toxic epidermal necrolysis and Stevens-Johnson syndrome are induced by soluble Fas ligand. Am J Pathol. 2003; 162(5):1515–1520.
[5] Fritsch PO, Ruiz-Maldonaldo R. Stevens-Johnson syndrome toxic epidermal necrolysis. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, et al., editors. Fitzpatrick's dermatology in general medicine. 5th ed. New York: McGraw-Hill. 1999; 644–654.
[6] Cisneros CG, Romiti R, Santi CG, Aoki V, Valente NY, et al. Toxic epidermal necrolysis-like cutaneous lupus erythematosus: A series of three patients. Acta Derm Venereol. 2010; 90(2):175–178.