Original Research
2014
September
Volume : 2
Issue : 3
Immunological study of cervical biopsy specimen for human papiloma virus
Surya Prabha V, Kanaka Bushanam GVVS, Sakuntaladevi G, Dharani Priya B
Pdf Page Numbers :- 145-148
Surya Prabha V1,2,*, Kanaka Bushanam GVVS3, Sakuntaladevi G2 and Dharani Priya B2
1Department Obstetrics & Gynaecology (O & G), Visakhapatnam Steel General Hospital (VSGH), Visakhapatnam, AP., India
2NRI Medical Hospital, Visakhapatnam, AP., India
3KIMS Foundation and Research Centre, Minister Road, Secunderabad - 500003, Telangana, India
*Corresponding author: Dr. V. Surya Prabha, MD., DGO., Assistant Professor, NRI Medical Hospital, Sangivalasa–531162, Bheemunipatnam (Mandal), Vishakapatnam (District), Andhra Pradesh, India. Email: dr.suryaprabha2011@gmail.com
Received 4 April 2014; Revised 15 May 2014; Accepted 12 June 2014
Citation: Surya Prabha V, Kanaka Bushanam GVVS, Sakuntaladevi G, Dharani Priya B. Analysis of HLA-A, HLA-B and HLA-DRB1 allelic frequencies in tertiary care from Andhra Pradesh. J Med Sci Res 2014; 2(3):145-148. DOI: http://dx.doi.org/10.17727/JMSR.2014/2-026
Copyright: © 2014 Surya Prabha V et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Cervical cancer is one of the most common cancers among women worldwide and its rates are higher in low and middle income countries. India is one not exemplified from the developing countries.
Aims: The main aim of the present work is a preliminary prospective screening study to observe the incidence of human papilloma virus (HPV) virus in the specimens of cervical biopsy taken from the patients of gynecology department of Visakha Steel General Hospital, RINL, Visakhapatnam district. Screening procedures like Pap smear, Colposcopy Immunohistochemistry (IHC) were done to identify the prevalence of HPV. It is an effort to assess and also improving the quality of cervical cancer prevention and treatment services in Visakhapatnam district of North coastal Andhra Pradesh.
Settings and design: This prospective study was conducted at the department of obstetrics and gynaecology, Visakha Steel General Hospital, RINL, Visakhapatnam district from January 2010 to December 2010.
Materials and methods: The Pap test and colposcopic examination were conducted on 161 patients and IHC was done on 24 cervical biopsy patients.
Results: The 87.58% of women was observed with abnormal Pap smear among that the severe dysplasia is around 10%. The abnormal cervix was seen by colposcopy is 89.44%. The 24 squamous metaplasia cases were subjected to IHC and 8 cases were found to be positive.
Conclusion: Pap smear, colposcopy along with cervical biopsy for HPV can provide enough information for an accurate diagnosis of cervical cancer and also from the future course of action for the treatment of the patients.
Keywords: cervical cancer; HPV; Pap smear; colposcope; IHC; screening
Full Text
Introduction
Globocan 2012 reveals striking patterns of cancer in women and highlights priority should be given to cancer prevention and control measures for breast and cervical cancers globally. According to this the cervical cancer is fourth most common cause of cancer death (266,000 deaths in 2011 and 500,000 new cases are reported) in women worldwide. In India cervical cancer is most frequent cancer in women. Current estimates are indicates 132,000 new cases diagnosed and 74,000 deaths annually in India [1-4].
Literature survey strongly supports HPV as the primary causal agent in development of cervical carcinoma [5-8]. At any given time, about 6.6% of women in the general population are estimated to harbor cervical HPV infection. Human papilloma virus can change normal cells to abnormal cells and they can turn into cancer cells if not detected early and treated. More than 150 exist; among only 30 types of HPV viruses are known to increase the risk of cervical cancer. The other 70 or so HPV types can cause infections and warts elsewhere on the body. Some "low-risk" types HPV 6 and HPV 11 cause genital warts which are not harmful and rarely associated with cervical cancers. "High-risk" HPV types 16 and 18 cause abnormal cell changes and which cause about 70% of all cervical cancers [9, 10].
Due to the dearth of population level screening programs to observe the prevalence of cervical carcinoma and its association to HPV in north coastal Andhra Pradesh has become main objective to choose present screening program in this particular area.
Material and methods
The cervical biopsy was taken from the age group between 18 to 45 years patients with the history of recurrent white discharge who were diagnosed as cervical erosion, chronic cervicitis, and also with family history of cancer cervix. Specimens were collected after preliminary investigations like hemoglobin percentage, bleeding time, clotting time, platelet count, blood sugar etc. Initial local infection was controlled with local antibiotics. Time of biopsy was fixed between 5th and 10th day after menstruation. Two specimens were collected separately in formalin bottle for fixation. One sample was subjected for Histo Pathological Examination (HPE) and another sample was subjected to immunohisochemical staining to observe HPV status. All examinations were conducted at the department of obstetrics and gynaecology, Visakha Steel General Hospital, RINL, Visakhapatnam district.
The principle behind the immunohistochemical staining method is a biotinylated secondary antibody forms a complex with peroxidase – conjugated streptavid molecules. Endogenous peroxidase activity is quenched by incubating the specimen for 5 minutes with 3% hydrogen peroxide. The specimen is then incubated with an approximately characterized and diluted mouse primary antibody, followed by sequential 10 minute incubations with a biotinylated link antibody (containing anti rabbit and anti-mouse immunoglobulins) and peroxidase-labelled streptavidin. Staining is completed after incubation with substrate chromogen. If the tissue stains brown indicates the specimen is positive for the disease.
Before taking biopsy Schiller’s test, acetic acid test and colposcopy were performed as a routine on cervix.
Results
The study was conducted to identify prevalence of HPV by IHC in the specimens of cervical biopsy. IHC assessment of the proliferative activity is very helpful to establish the diagnosis of pre neoplastic lesions of the cervix and also it is a simple one of the possible diagnostic parameter in the evaluation of the patients. This method is simple and cost effective in comparison to HPV DNA test.
A total of 161 patients were tested by Pap smear test before subjecting to biopsy. The primary method for detection of high-risk HPV is still the Papanicolaou-stained (Pap) smear. Since its introduction, the Pap smear has helped to reduce cervical cancer incidence and mortality rates. The Pap smear is a screening tool that looks for changes in cells of the transformation zone of the cervix. Often these changes are caused by HPV. The distribution of results of Pap smear test was shown in the Table 1. The 87.58% of women was observed abnormal Pap smear among that the severe dysplasia is around 10%. The cervical lesion and warts slider were shown in Figures 1 & 2.
Table 1: Observation of the abnormality by Pap smear.
|
S.No. .
|
Pap Smear
|
No
|
%
|
|
1.
|
NILM
|
20
|
12.42
|
|
2.
|
NILM
|
82
|
50.93
|
|
3.
|
LSIL
|
43
|
26.71
|
|
4.
|
HSIL
|
16
|
9.94
|
|
|
Total
|
161
|
100
|
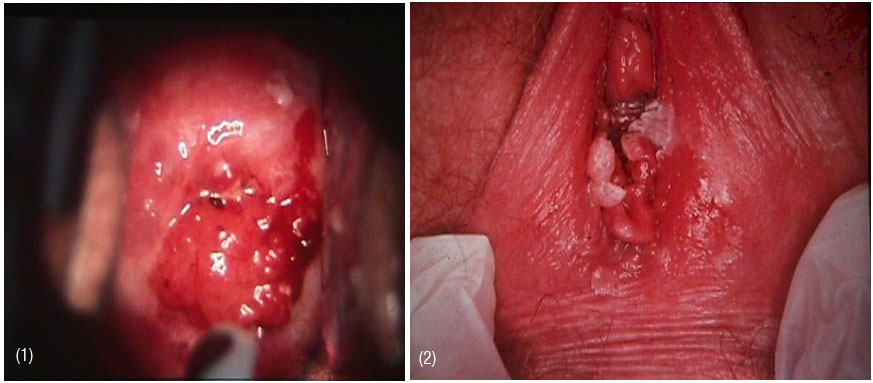
Figure 1: Cervical lesion, and
Figure 2: Warts.
The abnormal Pap smear results usually require further evaluation and it can be done with colposcopy. It magnifies the view 2 to 6 times for assessment of the size and margins of an abnormal transformation zone and determination of extension into the endocervical canal. The application of 3-5% acetic acid dissolves mucus and the acid’s desiccating action sharpens the contrast between normal and actively proliferating squamous epithelium. So, the colposcopic examination was conducted on total 161 subjects and results were given in the Table 2. The abnormal cervix was seen by colposcopy is 89.44% whereas with Pap smear it was 87.58%.
Table 2: The results of colposcopic observation among the patients.
|
S.No.
|
Colposcopy
|
No
|
%
|
|
1.
|
Normal
|
17
|
10.56
|
|
2.
|
Cervical cervitis
|
68
|
42.24
|
|
2.
|
Squamous metaplasia
|
24
|
14.91
|
|
3.
|
Polyp
|
4
|
2.48
|
|
4.
|
Aceto-White epithelium
|
15
|
9.32
|
|
5
|
Nebotheal follicle
|
09
|
5.59
|
|
6
|
Atrophy
|
2
|
1.24
|
|
7
|
Ulcer
|
1
|
0.62
|
|
8
|
Vascular abnoprmalities
(mosaicism, punctations, abnormal vessels)
|
18
|
11.18
|
|
9
|
Ectocervical cancer
|
2
|
1.24
|
|
10
|
Endocervical cancer
|
1
|
0.62
|
|
|
Total
|
161
|
100
|
All 24 squamous metaplasia cases were analysed for IHC. The results were interpreted with standard protocol. If the tissue was stained brown indicates that the slide was positive for HPV (Figure 3). In our study among the 24 cases HPV was found to be positive in 8 cases.
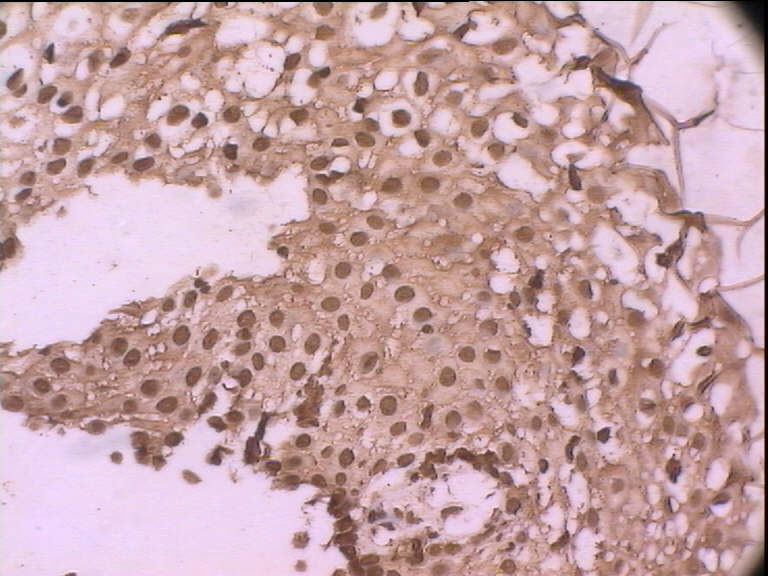
Figure 3: Brown staining of cervical cells by immunohistochemistry.
Discussion
Cervical cancer caused by HPV infection is one of the leading causes of cancer in Indian women. Though there are several screening methods available to screen but increasing cervical cancer incidence is due to lack of awareness among the high risk group, fear of diagnosing cancer among them and also lack of cost effective and available screening programs to detect precancerous conditions before they progress to invasive cancer. Various studies were supporting this condition [11-13].
In view of this particularly screening for cervical cancer by colposcopic evaluation was implemented systematically by the department of gynecology of Steel General Hospital in Visakhapatnam district under the aegis of first author in 1991 [14]. In the present work she has conducted preliminary work on IHC to observe the prevalence HPV among the squamous metaplasia cases (24) which were identified by colposcopic examination. Among that 33.33% (8) positive cases were observed.
Conclusion
Our study says next to Pap and colposcopic examinations more sensitive and low cost screening method is IHC method reliable for large scale screening of cervical cancer in India to identify the prevalence of HPV virus. Once HPV virus infection is addressed by the possible incidence of virus in the population, the prevention can be planned by vaccinating adolescence and reproductive age group women. It in turn reduces the morbidity and mortality rates dramatically in the population.
Acknowledgement
We are thankful to the Management of RINL for giving permission to carry out this project work in the Department of Obstetrics and Gynaecology, Visakha Steel General Hospital, Visakhapatnam.
Conflict of interest
The authors declare no conflict of interest.
References
1. Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11, Lyon, France: International Agency for Research on Cancer 2013.
2. Bray F, Ren JS, Masuyer E, Ferlay J. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer 2013; 132(5):1133–1145.
3. Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, et al. HPV screening for cervical cancer in rural India. N Engl J Med 2009; 360(14):1385-1394
4. WHO/ ICO Information Centre on HPV and Cervical Cancer (HPV information centre). Summary report on HPV and cervical cancer statistics in India 2007. (Available on 27 June 2014: http://www.hpvcentre.net/statistics/reports/IND.pdf)
5. Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J. Natl Cancer Inst. 1995; 87:796–802.
6. Singh N. HPV and Cervical cancer Prospects for prevention through vaccination. Ind J of Med Ped Oncol. 2005; 26(1):20–23.
7. Schiffman M, Castle PE, Jeronimo J, Rodriquez AC, Wacholder S. Human Papilloma virus and Cervical cancer. Lancet 2007; 370(9590):890–907.
8. Kartikeyan K. Cervical cancer in India and HPV virus Vaccination. Ind J of Med and Paed oncol. 2012; 33(1):7–12.
9. Gravitt PE, Lacey JV Jr, Brinton LA, Barnes WA, Kornegay JR, et al. Evaluation of self-collected cervicovaginal cell samples for human papillomavirus testing by polymerase chain reaction. Cancer Epidemiol Biomarkers Prev. 2001; 10(2):95–100.
10. Eileen M Burd. Human Papilloma Virus and Cervical cancer. Clinical Microbiology Reviews 2003; 16(1):1–17.
11. Dabash R, Vajpayye J, Jacob M, Dzuba I, Lal N, et al. Strategic assessment of cervical cancer prevention and treatment services in 3 districts of Uttar Pradesh, India. Reproductive health 2005; 2(11).
12. Sankarnarayanan R, Budukh AM, Raj Kumar R. Effective screening programmes for cervical cancer in low and middle income developing countries. Bulletin of WHO 2001; 79:954–962.
13. Sing N. HPV and Cervical cancer- prospects for prevention through vaccination. Ind J of Med Ped Oncol. 2005; 26(1):20–23.
14. Surya Prabha V, Dharani Priya B. Colposcope-A boon to detect precancerous condition. Ind J Multidiscip Res 2006; 2(2):183–188.