Original Research
2022
March
Volume : 10
Issue : 1
Factors affecting mortality in COVID-19 patients
Chikkahonnaiah P, Abdulla KK, Varshini J
Pdf Page Numbers :- 11-15
Prashanth Chikkahonnaiah1,*, Abdulla KK1, and Varshini J1
1Department of Respiratory Medicine, Mysore Medical College and Research Institute, Mysuru-570001, Karnataka, India
*Corresponding author: Dr Prashanth Chikkahonnaiah, Head of the Department, Department of Respiratory Medicine, Mysore Medical College and Research Institute, Mysuru-570001, Karnataka, India. Email: prshnthcr@gmail.com
Received 9 November 2021; Revised 13 December 2021; Accepted 17 December 2021; Published 27 December 2021
Citation: Chikkahonnaiah P, Abdulla KK, Varshini J. Factors affecting mortality in COVID-19 patients. J Med Sci Res. 2022; 10(1):11-15. DOI:http://dx.doi.org/10.17727/JMSR.2022/10-3
Copyright: © 2022 Chikkahonnaiah P et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Coronavirus disease 2019 (COVID-19) has caused large number of deaths all over the world. Our study was conducted to investigate the factors affecting mortality in patients hospitalized with COVID-19 during second wave of pandemic in India.
Material and methods: The data was collected retrospectively from the medical records of P. K. Trauma Care Centre, Mysuru where exclusively COVID-19 patients were admitted during second wave of COVID-19 pandemic in India. This study included total of 98 patients who expired due to COVID-19 during the period of March 2021 to October 2021. Demographic details, clinical presentation, treatment and laboratory data were extracted from medical records. We analysed the significance of the data using chi square test and other statistical tests.
Results: A total of 948 cases were admitted during the said period and 98 patients expired. With statistical analysis following factors are found to be significantly associated with high mortality - age above 60 years, unvaccinated, low oxygen saturation at presentation to the hospital, high serum ferritin level, elevated neutrophil –lymphocyte ratio (NLR), elevated D-dimer level, presence of co-morbidities. Duration of symptoms with which the patients presents to the hospital is the least significant factor associated with the mortality.
Conclusion: Elderly age group, lack of vaccination, low oxygen saturation at presentation to the hospital, presence of comorbidities like diabetes, hypertension and ischemic heart disease, elevated serum ferritin, D-dimer level and high NL ratio are associated significantly with high mortality in patients with COVID-19 infection. Vaccination, monitoring of oxygen saturation and proper management and control of comorbidities are the easily modifiable factors to reduce the mortality in COVID-19 patients.
Keywords: COVID-19; comorbidities; vaccination; mortality; SARS-CoV-2
Full Text
Introduction
Corona virus disease (COVID 19) is the infection caused by new virus among coronaviridae family namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a positive sense single stranded RNA virus which was first identified in the Wuhan city, China in 2019 December. As like SARS-CoV-1 virus, COVID-19 also spreads through droplet infection and there after it had become one of the largest pandemic affecting almost 200 countries and 7 continents worldwide, and more than 243 million people are affected with disease with more than 4.9 million deaths worldwide as per the data on October 2021 [1].
The pandemic began in 2019 and is still continuing world-wide with mutated variants of the SARS-CoV-2 virus. World Health Organization (WHO) classified these variants in to 4 variants of concern and 7 variants of interest. These variants are currently causing the pandemic in various countries with a change in mortality pattern. Cytokine storm is the main cause for death among infected individuals [2, 3]. The virus after entering into type 1 and 2 alveolar cell, activates macrophages, natural killer cells. Thus the innate immunity which is activated leads to progression of inflammation with release of cytokines and chemokines like interleukin–6, ferritin, fibrinogen, d-dimer, hepcidin, seerum amyloid A. This robust cytokine storm leads to ARDS and if left unchecked causes death of the patients [4, 5].
Most of the countries have gone through the second wave of the COVID-19 pandemic within 1.5 year of its origin and the large number of new cases and death were reported in second wave than first wave. India is also among one of the country largely affected by the COVID-19 with latest statistics says more than 3.4 crore people have been affected by COVID-19 and up to 4.5 lakh deaths were reported [6]. Studies conducted in various countries in first wave was showing that the mortality was high among old age and those with low immunity including co morbidities like diabetes, hypertension, ischemic heart disease etc [7–11]. But various reports from the countries affected in second wave was showing deaths even in young individuals without any co morbidities. So it is highly necessary to review various factors affecting the mortality in COVID patients.
Till December 2021, there was less number of studies which are published from India, especially from Karnataka state in second wave of the pandemic. Therefore, this study was planned to determine the factors affecting the mortality in COVID patients admitted at PKTCC Hospital, Mysore Medical College and Research Institute, Mysore, Karnataka.
Methods
Data collection
Study was conducted at Princess Krishnajammanni Trauma Care Center which was a designated COVID hospital during second wave of COVID-19. Institutional ethical committee clearance was taken. Data was collected from medical records of patients admitted from March 2021 to October 2021. Patients were referred from all over Mysore with either positive rapid antigen test or reverse transcription-polymerase chain reaction (RT-PCR). Totally 948 patients were admitted during the said period and 98 patients expired during the hospital stay. One patient was excluded from the study since his death was not directly related to COVID-19. We went through medical records and collected the demographic details, duration of symptoms, oxygen saturation at presentation, vaccination status, co morbidities and lab parameters including serum ferritin, D-dimer (COBAS6000 by immunoassay) level and neutrophil lymphocyte ratio (Sysmex). Patients were labelled as COVID-19 positive if they were positive in rapid antigen test or RT-PCR for SARS-CoV-2. 10 patients were both RAT and RT-PCR negative, but COVID-19 bronchopneumonia was confirmed by HRCT thorax (Siemens 128 slice CT machine) with expert opinion from Radiologist. We also went through chest x-ray (Skanray), CT thorax, ECG, vitals during admission, presence of co morbidities, presence of COVID-19 infection and COVID-19 related death in close contact family members.
Statistical analysis
Collected data were entered in Microsoft excel sheet and data were expressed as frequencies for categorical variables and as median for continuous variables. Continuous variables were also subdivided into groups and frequencies were matched. Significance of independent risk factors was analysed using logistic regression analysis. A comparison of variables between vaccinated and non-vaccinated groups were done using chi square test with help of a statistician. Statistical analysis was done using SPSS 21.0 and results were taken as significant if p values were less than 0.05.
Results
Study included 98 patients who expired in PKTCC, Mysuru during 2nd wave of COVID-19 from March 2021 to October 2021. One patient was excluded from the study as his death was not directly related to COVID-19 pneumonia. Factors which we have been taken into consideration includes age, gender, vaccination status, co morbidities, duration of symptoms at presentation to hospital, oxygen saturation at presentation to hospital, lab parameters like neutrophil-lymphocyte ratio, serum ferritin level, serum LDH level & D-dimer level at the time of presentation to the hospital (Figure 1 and Table 1). After stastical analysis using SPSS 21.0 results can be concluded as follows for each factors.
Out of 98 patients none of them were falling below 25 year of age, 48 patients (49%) were above 60 years of age and rest were falling in between 26 to 59 years of age. Out of these 48 patients of above 60 year 11 were vaccinated compared to only 2 patients were vaccinated among 26 to 59 year of age group. Even though statistically insignificant data points towards that geriatric age group are at higher risk of mortality due to COVID-19, and protective efficacy of vaccination may be hampered by low immunity of geriatric age group compared to other age group.
In this study, 60 patients (61.2%) were male and 38 were females (38.8%). 54 0ut of 60 males and 31 out of 38 females are not vaccinated in this study (Figure 2 and Table 2). Even though males has high mortality rate in this study it is statistically insignificant and not vaccinated is a statistically significant risk factor in both males and females.
In this study majority were not vaccinated. 85 patients (86.7%) were not vaccinated and 13 patients had received first dose and only 4 patients had received 2nd dose of vaccination. This study showed that those who are not vaccinated have higher risk of mortality than vaccinated individuals. And the values are statistically significant with p value less than 0.05. On analysing data in detail it is found that out of 13 patient expired despite vaccination,10 were having co morbidities (7 had diabetes, 2 had ischemic heart disease and 1 had hypertension) and rest of the 3 were above 60 years of age. All the patients below 50 years of age, who expired, were not vaccinated (Figure 2 and Table 2).
Almost 43.9% has presented to hospital within 4 days of onset of symptoms and 50% patients visited hospital with in 5 to 10 days of onset of symptoms. Only 6.1% patients presented later than 10 days of onset of symptoms. This study suggests that duration of symptoms with which patient presented to hospital is not significantly associated with mortality and this study suggests that almost half of the patients appreciate first symptoms only after disease progresses to moderate to severe disease.
In this study 83 patients out of 98 (86.5%) had visited hospital with oxygen saturation less than 90% (severe COVID pneumonia as per Ministry Of Health and Family Welfare, India guidelines) and 11 patients presented with oxygen saturation between 90-94% (moderate disease as per, Ministry Of Health and Family Welfare India guidelines) and only 2 patients has presented with oxygen saturation >94%. This study shows that low oxygen saturation at presentation is significantly associated with high mortality with p value <0.05. This study suggests that daily monitoring of oxygen saturation is highly important in COVID-19 pneumonia to reduce the mortality.
Diabetes mellitus (45%), hypertension (32%), Ischemic heart disease (10%), chronic kidney disease (4%) and hypothyroidism (6%) were the co morbidities found with the patients in this study. Diabetic and hypertensive patients had highest mortality than any other co morbid conditions. Diabetes mellitus is associated with high mortality even in vaccinated group.
Most of the patients were found to have elevated levels of serum ferritin, Neutrophil –lymphocytic ratio and elevated level of D-dimer. Even though it is statistically insignificant serum ferritin levels are elevated >1000 in non-vaccinated individual than vaccinated individual. Totally 86% were found to have elevated serum ferritin level and 92% had elevated NL ratio irrespective of vaccination status. From the retrospective analysis of hospital records we got only 17 patients with recorded level of D-dimer, out of that 13 had elevated levels of D-dimer (76.4%). Elevation of individual parameters is statistically significant. Other parameters which was statistically significant was presence of chest x-ray lesion. All the patients (100%) had presence of consolidation in lung fields at the time of admission with most common presentation being bilateral lower zone consolidation.
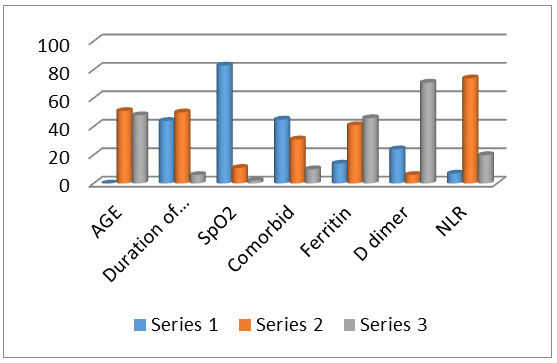
Figure 1: Comparison of parameters associated with mortality in COVID -19.
Table 1: Series classification of figure 1.
|
|
Series 1
|
Series 2
|
Series 3
|
|
Age
|
<25 years
|
26-59 years
|
>60 years
|
|
Duration of symptoms
|
<4 days
|
5 -10 days
|
>10 days
|
|
SpO2 at presentation
|
<90%
|
91- 93%
|
>94%
|
|
Comorbidities
|
Diabetes
|
Hypertension
|
Ischemic heart disease
|
|
Ferritin
|
<250 IU/ml
|
251-999
|
>1000
|
|
D–dimer
|
<0.5 ng/ml
|
0.6-0.9
|
>1
|
|
NLR
|
<3.5
|
3.6-16.9
|
>17
|
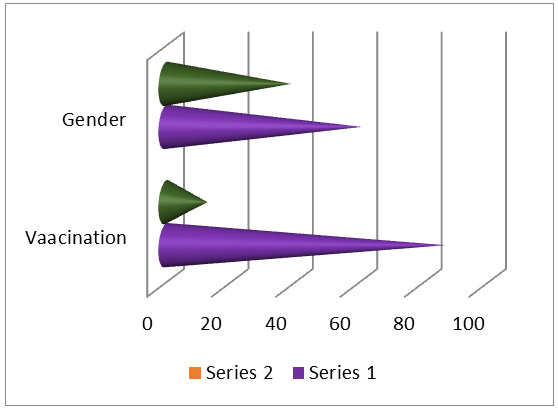
Figure 2: Comparison of gender and vaccination status in COVID-19 mortality.
Table 2: Series classification of figure 2.
|
|
Series 1
|
Series 2
|
|
Gender
|
Male
|
Female
|
|
Vaccination
|
No
|
Yes
|
Discussion
Our study has investigated regarding factors affecting the mortality in patients hospitalised with COVID-19. Records of 98 patients expired from COVID-19 in second wave were retrieved and data collected.
As like other studies this study also shows that there is no significant relationship with gender and the death [12]. Both males and females are affected. But in few large scale study conducted mortality rate was high in males than in females [11, 13]. This study showed death was more common in elderly age group and the risk increases after the age of 60 year. This correlates with various other studies which also shows median age of died patients was 63 year [14].
Vaccination status and oxygen saturation at the time of presentation to the hospital is found to be the most important factor affecting the mortality in this study. There are only few published studies which show effect of vaccination in COVID-19 mortality. As like this study where 87% patients were not vaccinated, various other available study also shows that oxygen dependence and death were significantly more common in non-vaccinated individuals [15]. Report published by Washington state department of health shows that there is 15 times more risk of mortality in non-vaccinated elderly COVID-19 patients compared to vaccinated individuals. In this study 86.5% had saturation less than 90% while presented to hospital. This correlates with other studies as well and it indicates development of hypoxia is the most important predictor of poor prognosis in COVID-19 patients as 13 patients in this study had received first dose of vaccination and 4 out of them had received even second dose of vaccine, but all of them had presented to the hospital with hypoxia.
Presence of comorbidities like diabetes and hypertension are found significantly associated with high mortality in this study. Diabetes is found to be significantly associated with need for ICU admission and high mortality in other studies, but hypertension was not found significant in some studies [14]. Presence of malignancies was found to be significantly associated with elevated D-dimer and high mortality in few studies [16], but in our study none of them had documented malignancy.
Lab parameters like high NLR, elevated serum ferritin and D-dimer level also found as significant factor which can predict the high mortality in COVID-19 patients. Increased neutrophil lymphocyte ratio indicates systemic inflammation and found to have prognostic value in various pathological condition and in community acquired pneumonia [17, 18]. There are also studies which shows lymphopenia has poor prognostic value in COVID-19 patients [19]. So high NLR indicates poor prognosis in severe COVID-19 pneumonia. But presence of high NLR in mild cases also reported from an another study conducted from PK Trauma care centre, Mysuru. Hence presence of high NLR per se does not indicate high mortality, but high NLR in patients admitted in COVID ICU indicates poor prognosis. Elevated levels of D-dimer is significantly associated with increased mortality rate, hence anticoagulant therapy was one of the essential treatment in moderate to severe COVID-19 patients in various guidelines including MOHFW guidelines by government of India [20]. In this study among documented cases 76% had elevated levels of D-dimer which correlates with other study as well [21]. Serum ferritin is considered as marker of inflammation and it is found elevated in COVID-19 patients. In this study 86% had elevated levels of serum ferritin at the time of admission to the hospital and more than half of them had significantly higher levels of serum ferritin more than 1000 ng/ml. Study conducted in Mexico and China also shows similar findings with respect to serum ferritin levels in severe COVID-19 pneumonia [21, 22].
In this study we have even compared significance of these factors in vaccinated and non-vaccinated groups among died patients. None of the older studies found doing the same in previous literature. The result was factors like elderly age group, low oxygen saturation, presence of diabetes mellitus, high NLR and elevated serum ferritin does not significantly differ in vaccinated and non-vaccinated groups, suggests that in all died patients with severe COVID-19 pneumonia irrespective of the vaccination status NLR and serum ferritin levels were elevated and most of them were elderly age group, presented with low oxygen saturation and diabetes was the most common comorbid condition in patients who have died due to severe COVID-19 disease irrespective of vaccination status. This finding has to confirm in further studies.
Study limitations
Major limitation of the study was small sample size. Also since this was a tertiary care center with majority of the patients admitted with severe COVID, identification of patients at risk for progression to severe disease could not be assessed.
Conclusion
From this study we have done retrospectively in 98 patients who have died of COVID-19 infection during the period of March 2021 to October 2021. We conclude that lack of vaccination, elderly age group, low oxygen saturation at presentation to hospital, comorbidities like diabetes and hypertension are significantly associated with high mortality in COVID-19 infected patients. High serum ferritin level, elevated D-dimer and neutrophil-lymphocytic ratio also indicates high mortality among COVID patients. Whereas factors like elderly age group, high serum ferritin, NL ratio does not significantly differ in vaccinated and non-vaccinated groups.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Weekly epidemiological update on COVID-19. Available on 26 October 2021 from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-COVID-19---26-october-2021
[2] Tang Y, Liu J, Zhang D, Xu Z, Ji J, et al. Cytokine Storm in COVID-19: The current evidence and treatment strategies. Front Immunol. 2020; 11:1708.
[3] Hojyo S, Uchida M, Tanaka K, Hasebe R, Tanaka Y, et al. How COVID-19 induces cytokine storm with high mortality. Inflamm Regen. 2020; 40:37.
[4] Carubbi F, Salvati L, Alunno A, Maggi F, Borghi E, et al. Ferritin is associated with the severity of lung involvement but not with worse prognosis in patients with COVID-19: data from two Italian COVID-19 units. Sci Rep. 2021; 11(1):4863.
[5] Qeadan F, Tingey B, Gu LY, Packard AH, Erdei E, et al. Prognostic values of serum ferritin and D-dimer trajectory in patients with COVID-19. Viruses. 2021; 13(3):419.
[6] India Situation Report. Accessed from internet.
[7] Laxminarayan R, Mohan CB, Vinay TG, Kumar KVA, Wahl B, et al. SARS-CoV-2 infection and mortality during the first epidemic wave in Madurai, south India: a prospective, active surveillance study. Lancet Infect Dis. 2021; 21(12):1665–1676.
[8] Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nature Reviews Cardiology. 2020; 17:543–558.
[9] Li X, Xu S, Yu M, Wang K, Tao Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020; 146(1):110–118.
[10] Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020; 108:154262.
[11] Bağ Soytaş R, Ünal D, Arman P, Suzan V, Emiroğlu Gedik T, et al. Factors affecting mortality in geriatric patients hospitalized with COVID-19. Turk J Med Sci. 2021; 51(2):454–463.
[12] Sun H, Ning R, Tao Y, Yu C, Deng X, et al. Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: A retrospective study. J Am Geriatr Soc. 2020; 68(6):E19–23.
[13] Yu C, Lei Q, Li W, Wang X, Liu W, et al. Clinical characteristics, associated factors, and predicting COVID-19 mortality risk: a retrospective study in Wuhan, China. Am J Prev Med. 2020; 59(2):168–175.
[14] Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in lombardy, Italy. JAMA Intern Med. 2020; 180(10):1345–1355.
[15] Hippisley-Cox J, Coupland CA, Mehta N, Keogh RH, Diaz-Ordaz K, et al. Risk prediction of COVID-19 related death and hospital admission in adults after COVID-19 vaccination: national prospective cohort study. BMJ 2021; 374:n2244.
[16] Meng Y, Lu W, Guo E, Liu J, Yang B, et al. Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: a propensity score-matched analysis. J Hematol Oncol. 2020; 13:75.
[17] Huang H, Wan X, Bai Y, Bian J, Xiong J, et al. Preoperative neutrophil-lymphocyte and platelet-lymphocyte ratios as independent predictors of T stages in hilar cholangiocarcinoma. Cancer Manag Res. 2019; 11:5157–5162.
[18] Cataudella E, Giraffa C, Marca S, Pulvirenti A, Alaimo S, et al. Neutrophil-to-lymphocyte ratio: an emerging marker predicting prognosis in elderly adults with community-acquired pneumonia. J Am Geriatr Soc. 2017; 65(8):1796–1801.
[19] Liu Y, Du X, Chen J, Jin Y, Peng L, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020; 81(1):e6–12.
[20] Varghese GM, John R, Manesh A, Karthik R, Abraham OC. Clinical management of COVID-19. Indian J Med Res. 2020; 151(5):401–410.
[21] Vargas-Vargas M, Cortés-Rojo C. Ferritin levels and COVID-19. Rev Panam Salud Pública. 2020; 44:e72.
[22] Marimuthu AK, Anandhan M, Sundararajan L, Chandrasekaran J, Ramakrishnan B. Utility of various inflammatory markers in predicting outcomes of hospitalized patients with COVID-19 pneumonia: A single-center experience. Lung India. 2021; 38(5):448–453.