Orginal Research
2023
March
Volume : 11
Issue : 1
Effectiveness of antihypertensive agents in stage I/II hypertensive patients with ace (I/D) gene polymorphism
Bansal G, Chaithanya TM, Alam MA, Manchi RK
Pdf Page Numbers :- 22-25
Garima Bansal1, Thota Madhu Chaithanya2, Md Amir Alam3, and Rajesh Kumar Manchi4,*
1Department of Pharmacology, Pacific Medical College and Hospital, Pratappura, Udaipur- 313001, Rajasthan, India
2Department of Pharmacology, Saraswati Medical College, Madhuvihar, Ashakhera, Unnao, Uttar Pradesh-209859, India
3Department of Pharmacology, RKDF Medical College Hospital & Research Center & Hospital, Bhopal-462026, Madhya Pradesh, India
4Department of Pharmacology, Lord Buddha Koshi Medical College & Hospital, Baijnathpur, Saharsa - 852221, Bihar, India
*Corresponding author: Dr. Rajesh Kumar Manchi, Associate Professor, Department of Pharmacology, Saraswati Medical College, Madhuvihar, Ashakhera, Unnao, Uttar Pradesh-209859, India. Email: manchirajesh1985@gmail.com
Received 21 September 2022; Revised 19 November 2022; Accepted 2 December 2022; Published 12 December 2022
Citation: Bansal G, Chaithanya TM, Alam MA, Manchi RK. Effectiveness of antihypertensive agents in stage I/II hypertensive patients with ace (I/D) gene polymorphism. J Med Sci Res. 2023; 11(1):22-25. DOI: http://dx.doi.org/10.17727/JMSR.2023/11-5
Copyright: © 2023 Bansal G et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Angiotensin converting enzyme (ACE) is the key enzyme, regulates the blood pressure which is encoded by 21kb gene that consists of 26 exons and is located on chromosome 17, contains a polymorphism in the form of either Insertion (I) or Deletion (D). The aim was to study the effect of antihypertensive drugs in patients of essential hypertension associated with ACE gene polymorphism.
Methods: Hypertensive patients were recruited followed by genetic test was done for detecting ACE gene polymorphism, then patients were divided as Group-A & B. Group –A and B patients were treated with atenolol (25mg) and azilsartan (40 mg) for three months respectively.
Results: Systolic and diastolic blood pressure was recorded in both the groups before and after commencement of treatment. Among 88 patients of newly diagnosed hypertension, majority of study population belongs to genotype D/D (38.63%) followed by I/D (31.81%) and II (29.54%) genotype. Significant difference was found in systolic blood pressure (p<0.05) of both groups but not diastolic blood pressure (p>0.05).
Conclusion: The rate of control of blood pressure was high in I/I genotype followed by D/D genotype irrespective of treatment group. Overall better prognosis was observed with azilsartan 40mg compared to atenolol 25mg treatment in patients with ACE gene polymorphisms.
Keywords: hypertension; ACE gene; azilsartan; atenolol; pharmacogenetics
Full Text
Introduction
Hypertension (HTN) or high blood pressure, sometimes called arterial hypertension, is a chronic medical condition in which the blood pressure in the arteries is elevated. According to WHO (2019), hypertension is an interesting disease entity of its own. As it remains silent, being generally asymptomatic during its clinical course, the disease does immense harm to the body in the form of ‘Target Organ’ damage; hence, the WHO has named it the ‘Silent Killer’ [1]. It is a major cause of morbidity and mortality because of its association with coronary heart disease, cerebrovascular disease and renal [2].
The global prevalence of hypertension has been increasing. Recent studies from India have shown the prevalence of hypertension to be 25% in urban and 10% in rural adults in India [3]. In India by the end of 2025 the projected prevalence of hypertension men and women are 22.9% and 23.6% as per the statistics of directorate general of health services, ministry of health & family welfare, Government of India.
The angiotensin converting enzyme (ACE) is encoded by 21kb gene that consists of 26 exons and is located on chromosome 17 and contains a polymorphism in the form of either Insertion (I) or Deletion (D) of a 287-base pair allele repetitive sequence in introns. The polymorphism is shown to be associated with the interpersonal variability and individuals carrying the Deletion allele are associated with increased ACE levels [4]. This ACE enzyme is able to cleave proteins. It is part of the renin-angiotensin system, which regulates blood pressure and the balance of fluids and salts in the body.
Various studies have illustrated the association between ACE I/D polymorphism and cardiovascular complications [5, 6], but the association between I/D polymorphism and hypertension is still controversial. Some studies have shown the association of ACE I/D polymorphism with essential hypertension [7, 8] and some studies were failed to show the association [9, 10]. Renin-angiotensin-aldosterone system (RAAS) regulates the blood pressure along with electrolyte balance [11]. The level of mean plasma ACE high in DD subjects than II subjects. Mean plasma ACE levels are high in DD subject followed by ID and then II subjects [12, 13].
The present study aimed to explore the association between ACE gene(I/D) polymorphism and essential hypertension in north Indian population.
Materials and methods
The study is non-randomized, prospective control clinical trial, conducted in Department of Pharmacology in collaboration with Department of General Medicine, Rama Medical College Hospital & Research Center, Kanpur. Study was started after getting approval from institutional ethical committee. Informed concern was obtained from each patient before starting present study. Patients were recruited as per inclusion criteria given below.
The inclusion criteria were (a) Patients with systolic blood pressure more than 120-139 mm Hg and diastolic blood pressure 80-89 mm Hg, (b) Patients with age group of 30-50 years from both sexes, (c) Who are willing to give informed consent.
The exclusion criteria were (a) Smokers/ alcoholics /Pregnant & lactating women, (b) Complicated hypertension, (c) Patients with psychiatry, liver, kidney, cardiac problems and also chronic infections like TB, leprosy, recent trauma, surgery, (d) Hypersensitivity to any of study drugs, (e) Patients who are unwilling to participate and give informed consent or mental incapacity to take the drug.
Isolation of DNA: The DNA was extracted by salting out method using Qiagen Kit. DNA quality was estimated with the use of 1% agarose gel electrophoresis and the quality of DNA was also calculated with the use of standard spectrophotometer at 260 nm and 280 nm ratio.
ACE gene polymorphism by polymerase chain reaction: To determine the ACE gene genotype (SNP rs4343) of cases of newly diagnosed hypertensive patients, the genomic DNA fragments were amplified by PCR.
Following primers were used to detect gene presence and followed by polymorphism.
Forward Primer: 5’-CTGGAGACCCCCATCCTTTCT-3’ Tm=56.00oC
Reverse Primer: 5’-GATGTCGCCATCACATTCGTCAGAT-3’ Tm=57.56oC
The PCR conditions were 95oC for 3min, 35 cycles of 95oC for 30s, 52oC for 30s, 72o C for 1.20 min and final extension at 72oC for 5min.
As per inclusion and exclusion criteria a total of 88 newly diagnosed hypertension patients were enrolled for the study. 5ml of venous blood was collected from each patient followed by genetic test was done for detecting ACE gene polymorphism, then the patients were divided into two groups, Group-A and Group-B. Both the groups were treated for 3 months as follows:
Group-A: (n=44) patients received atenolol (25 mg/day)
Group-B: (n=44) patients were given azilsartan (40 mg/day)
At the beginning of study demographic data along with patient past medical history was taken and followed by venous blood collected and stored until genetic test is done. DNA was extracted from whole blood containing EDTA by salting out method. Basic investigations for blood pressures (systolic and diastolic) were done at beginning and after three months of study. This study had 6 months follow-up’s which were scheduled after every 15 days. At every follow-up general medical condition was assessed and investigations for blood pressure (systolic and diastolic) were done. Blood pressure was estimated by auscultatory method using sphygmomanometer.
Statistical analysis
Data was analyzed using ‘Unpaired’ test and results were expressed as mean ± standard deviation (SPSS 20 software).
Results
Among 88 patients of newly diagnosed hypertension, 42(47.72%) patients were females and 46(52.27%) were males and 61(69.31%) patients belongs to age group between 46 to 55 years, 11(12.5%) patients belongs to age group between 56 to 65 years and 16(18.18%) patients age was between range of 36 to 45 years (Table 1).
Table 1: Gender and age distribution of study population.
|
Variables
|
n = 88
|
|
Gender
|
Females
|
42(47.72%)
|
|
Males
|
46(52.27%)
|
|
Age range
|
36-45 years
|
16(18.18%)
|
|
46 -55 years
|
61(69.31%)
|
|
56– 65 years
|
11(12.5%)
|
The frequency of I/D allele was more as compared with I/I and D/D allele (Table 2).
Table 2: Distribution of genotypes among study population.
|
Genotype
|
Group-A
|
Group-B
|
|
I/I genotype
|
13(29.54%)
|
13(29.54%)
|
|
I/D genotype
|
14(31.81%)
|
14(31.81%)
|
|
D/D genotype
|
17 (38.63%)
|
17(38.63%)
|
According to the gel photograph to the sequence we obtained II allele was observed at 421bp and ID allele was observed at 200bp and DD band was observed at 50bp. There were 3 types of genotypes seen in the ACE gene polymorphism: II homozygous, ID heterozygous and DD homozygous (Figure 1).
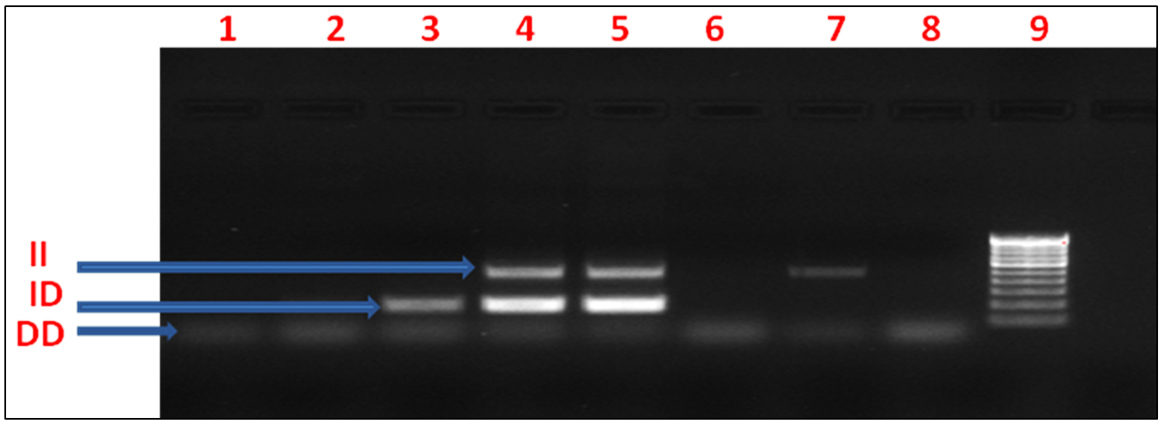
Figure 1: PCR product digested with restriction fragment length polymorphism (RFLP).
After 3 months of treatment with atenolol (Group-A) and azilsartan (Group-B) baseline values were compared with 3rd month values, there was significant reduction in mean systolic and diastolic blood pressure observed in both group-A and group-B, but high reduction in mean systolic blood pressure was observed in azilsartan treated group (Group-B) as compared with atenolol treated group (Group-A), which is statistically significant (p<0.05) (Table 3) but there was no statistical difference found in mean diastolic blood pressure when both groups were compared at 3rd month treatment (Table 4).
Table 3: Comparison of systolic blood pressure (mmHg) in atenolol versus azilsartan ACE gene positive group.
|
Genotype
|
Atenolol
|
Azilsartan
|
Mean difference+ SD
|
P value
|
|
Baseline
|
I/I
|
164.72±6.14
|
162.30±6.36
|
2.41±2.56 (95% CI -2.90 to 7.74)
|
P>0.356ns
|
|
I/D
|
166.12±4.97
|
166.62±4.99
|
-0.5±1.76 (95% CI -4.09 to 3.09)
|
P>0.779 ns
|
|
D/D
|
166.92±4.43
|
166.28±5.07
|
0.64±1.45 (95% CI -0.85 to 5.0)
|
P>0.160 ns
|
|
3 months
|
I/I
|
130.18±3.02
|
126.92±4.59
|
3.25±1.62 (95% CI- 0.10 to 6.62)
|
P<0.001**
|
|
I/D
|
136.62±3.07
|
132.25±2.04
|
4.37±0.92 (95% CI- 2.48 to 6.26)
|
P<0.03**
|
|
D/D
|
138.18±3.20
|
134.19±3.89
|
3.9±1.08 (95% CI- 1.80 to 6.18)
|
P<0.05**
|
Note: Significant: p- value<0.05*
Table 4: Comparison of diastolic blood pressure (mmHg) in atenolol versus azilsartan gene positive patients.
|
Genotype
|
Atenolol
|
Azilsartan
|
Mean difference ± SD
|
P-value
|
|
Baseline
|
I/I
|
98.18±2.44
|
100.76±5.62
|
-2.58±1.83 (95% CI -6.2 to 1.05)
|
P>0.152ns
|
|
I/D
|
98.62±4.11
|
102.25±3.64
|
-0.5±1.76 (95% CI -4.09 to 3.09)
|
P>0.071 ns
|
|
D/D
|
100.18±4.13
|
102.85±4.45
|
-2.67±1.30 (95% CI -5.3to 0.29)
|
P>0.158 ns
|
|
3 months
|
I/I
|
82.36±2.33
|
84.76±3.60
|
-2.4±1.26 (95% CI- 3.02 to 0.22)
|
P>0.071 ns
|
|
I/D
|
84.50±3.05
|
86.25±4.55
|
-1.75±1.37 (95% CI 4.54 to 1.04)
|
P>0.212 ns
|
|
D/D
|
88.36±4.07
|
88.38±4.17
|
-0.017±1.25 (95% CI- 2.55 to 2.56)
|
P>0.989 ns
|
Note: Significant: p- value <0.05**.
Discussion
ACE gene polymorphism elevates plasma level of ACE which is associated with rise in blood pressure. Renin-Angiotensin-Aldosterone-System (RAAS) is one of the regulatory systems governing circulation, systemic vascular resistance, and kidney function. RAAS activity is directly proportional to blood pressure [14]. If hypertension is left untreated it predisposes to coronary artery disease (CAD), left ventricular hypertrophy (LVH), congestive heart failure (CHF), chronic kidney diseases (CKD), end - stage renal disease (ESRD), transient ischemic attacks (TIA), and cerebrovascular accidents (CVA) [15].
Among 88 patients of newly diagnosed hypertension, 52.27% of study population was males and 47.72% was females, which is in line with findings of another study [16]. Majority of study population in present study i.e. 61% belongs to age group between 46 to 55 years, followed by 18.18% belongs to 36 to 45 years of age group, these findings are supported by another study [16]. Majority of study population belongs to genotype D/D followed by I/D genotype, same way of genotype distribution was found in another study [17, 18], but sample size is different from present study. Strong association was found between D allele and hypertension which is in line with previous study [18].
All the genotypes of both Group-A (Atenolol) and Group-B (Azilsartan) had shown significant reduction of systolic and diastolic blood pressure at the end of treatment, but when Group-A and B were compared, the significant difference was found in systolic blood pressure (p<0.05) but not diastolic blood pressure (p>0.05), similar results were found in another study but which was not genetic study [19].
Limitations
Sample size of present study is less hence it will be a premature decision to generalize the findings of present study, so multi-centric study involving various geographical areas and with different genetic races will be the better way to confirm the present results.
Conclusion
The frequency of D/D allele was more in study population followed by D/I and I/I allele. Blood pressure was high in D/D genotype followed by D/I genotype, whereas I/I genotype patients were having blood pressure less as compared to D/D and D/I genotype, so which conclude that D allele playing pathogenic role. Better prognosis was observed in patients treated with azilsartan as compared with atenolol irrespective of genotype. Better blood pressure control was seen in I/I genotype followed by D/I genotype and D/D genotype irrespective of antihypertensive being prescribed.
Acknowledgement
The Department of Pharmacology.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Badaruddoza AJS, Bhanwer AJS, Sawhney R, Randhawa NK, Matharoo K, et al. A study of Angiotensin Converting Enzyme (ACE) gene polymorphism in essential hypertension among a business community in Punjab. Int J Hum Genets. 2009; 9:231–234.
[2] Fornage M, Amos CI, Kardia S, Sing CF, Turner ST, et al. Variation in the region of the angiotensin-converting enzyme gene influences interindividual differences in blood pressure levels in young white males. Circulation. 1998; 97:1773–1779.
[3] Sehajpal P, Gupta S, Agrawal B, Goel R. Angiotensin-converting enzyme gene polymorphism in hypertensive rural population of Haryana, India. J Emerg Traum, Shock. 2009; 2:150.
[4] Kunz R, Bork JP, Fritsche L, Ringel J, Sharma AM. Association between the angiotensin-converting enzyme-insertion/deletion polymorphism and diabetic nephropathy: a methodologic appraisal and systematic review. J Amer Soc Nephrol. 1998; 9:1653–1663.
[5] Krishnan R, Sekar D, Karunanithy S, Subramanium S. Association of angiotensin converting enzyme gene insertion/deletion polymorphism with essential hypertension in south Indian population. Gene Diseas. 2016; 3:159–163.
[6] Munshi A, Sultana S, Kaul S, Reddy BP, Alladi S, et al. Angiotensin-converting enzyme insertion/deletion polymorphism and the risk of ischemic stroke in a South Indian population. J Neurol Sci. 2008; 272:132–135.
[7] Das M, Pal S, Ghosh A. Angiotensin converting enzyme gene polymorphism (Insertion/Deletion) and hypertension in adult Asian Indians: A population-based study from Calcutta, India. Hum Biol. 2008; 80:303–312.
[8] Mastan S, Nunn J. Angiotensin-converting enzyme deletion polymorphism is associated with hypertension in a Sikh population. Hum Hered. 1997; 47:250–253.
[9] Ashavaid TF, Shalia KK, Nair KG, Dalal JJ. ACE and AT1R gene polymorphisms and hypertension in Indian population. J Clin Labor Anal. 2000; 14:230–237.
[10] Chowdhury AH, Zaman MM, Haque KM, Rouf MA, Shah AT, et al. Association of angiotensin converting enzyme (ACE) gene polymorphism with hypertension in a Bangladeshi population. Bangladesh Med Res Coun Bull. 1998; 24:55–59.
[11] Corvol P, Soubrier F, Jeunemaitre X. Molecular genetics of the renin-angiotensin-aldosterone system in human hypertension. Pathologie-Biologie. 1997; 45:229–239.
[12] Rigat B, Hubert C, Alhenc-Gelas F, Cambien F, Corvol P, et al. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest. 1990; 86:1343–1346.
[13] Tiret L, Rigat B, Visvikis S, Breda C, Corvol P, et al. Evidence, from combined segregation and linkage analysis, that a variant of the angiotensin I-converting enzyme (ACE) gene controls plasma ACE levels. Amer J Hum Genet. 1992; 51:197–205.
[14] Kumar A, Mohindru K, Sehajpal PK. Angiotensin-I converting enzyme polymorphism and diabetic nephropathy in north India. Int J Hum Genet. 2005; 5:279–283.
[15] Mitch WE. Is the inherited ACE genotype a trump or a joker? J Clin Invest. 1995; 96:2100–2101.
[16] Benetos A, Safar M, Rudnichi A, Smulyan H, Richard JL, et al. Pulse pressure. Hypertension. 1997; 30:1410–1415.
[17] Malard L, Kakinami L, Loughlin J, Roy-Gagnon MH, Labbe A, et al. The association between the angiotensin-converting enzyme-2 gene and blood pressure in a cohort study of adolescents. BMC Med Genet. 2013; 14:117.
[18] Morshed M, Khan H, Akhteruzzaman S. Association between angiotensin i-converting enzyme gene polymorphism and hypertension in selected individuals of the Bangladeshi Population. BMB Reports. 2002; 35:251–254.
[19] Rahman F, Muthaiah N, Kumaramanickavel G. Current concepts and molecular mechanisms in pharmacogenetics of essential hypertension. Ind J Pharmacol. 2021; 53:301–309.