Full Text
Orthopaedic surgeries are included in high-risk group for development of deep vein thrombosis (DVT). This fear has induced many treating physicians to put the patient on prophylactic anticoagulant therapy, who are undergoing major lower limb orthopaedic surgeries, like total hip arthroplasty and total knee arthroplasty. Since there is paucity of Indian data regarding the extent to which patients are affected with DVT, the study was aimed to assess, by using color doppler, the incidence of DVT in patients following hip and knee arthroplasty.
Materials and methods
This is a prospective observational study (non-funded) to know the incidence of DVT and to analyze the associated risk factors in patients who underwent hip and knee arthroplasty surgery at Sri Ramachandra University, Chennai during the period April 2007 to August 2009.
Total number of patients included in the study was 99 out of which 5 were lost to follow-up. Of 94 patients 45(47.9%) were males and 49(52.1%) females. (a) The age distribution of the patients showed as follows, 3(3.2%) patients below 40 years, 14(14.9%) patients in the age group 41-50, 17(18.1%) patients in the age group 51-60, 34(36.2%) patients in the age group 61-70 and 26(27.7%) patients above 70 years age. (b) Amongst 94 patients, 23(24.5%) underwent total hip replacement, 25(26.6%) underwent hemiarthroplasty and 46(48.9%) underwent total knee replacement. The cases done by 6 surgeons were included. Some of the patients were given thromboprophylaxis based on the Surgeon's preference (protocol - injection enoxaparin, 40 mg once daily subcutaneously for 10 days).
In our study detailed history of all the patients was taken and all the patients were evaluated clinically every day for DVT during the stay in the hospital. The duration of follow-up was six weeks. Color doppler was done preoperatively, early postoperatively between the 5-13 day and late postoperatively between the 28-42 day i.e. 4-6 week postop during routine follow-up.
Statistical analysis
Results were analyzed using SPSS for windows software (v15). Independent Student’s t-test for continuous data and chi-square test for categorical data was used. Results were expressed as incidence, percentage or mean with standard deviation of the data and a significance level of p<0.05 was used. The sample size was calculated with alpha = 0.05 and power (1-alpha)=0.80. The sample we collected was found to be adequate according to the norms and analysis was done immediately after data collection.
Results
The incidence of DVT is 6.4% in this study.
Demographic distribution and incidence of DVT
In this study amongst 94 patients 45(47.9%) were males while 49(52.1%) were females. The series had a higher incidence of DVT amongst females-8.2%. 50% of the patients who developed DVT were in the age group of >70 years. The mean age of the patients in the study was 63 years (Min-36 years and max-84 years). 83.33% of the patients who developed DVT had undergone hip arthroplasty when compared to total knee replacement.
In the study the common indication for hip arthroplasty was fracture neck of femur (47.9%). The patients who had hip arthroplasty for fracture neck of femur showed higher incidence of DVT-4 out of 23(17.4%) but it was not found to be statistically significant. The mean age of the patients who underwent hemiarthroplasty was 72.8 years and that of THR was 56.35 years (Table 1). The incidence of DVT was found to be highest in the hemiarthroplasty group with higher mean age which was found to be significant (p<0.05) (Table 1).
Table 1: Mean age of the patients.
|
Surgery
|
No. of patients
|
Mean age
(in years)
|
Standard deviation
|
DVT positive
|
p value
|
|
THR
|
23(24.5%)
|
56.35
|
12.82
|
1(4.3%)
|
p<0.05
|
|
HEMI
|
25(26.6%)
|
72.80
|
9.22
|
4(16%)
|
|
TKR
|
46(48.9%)
|
61.78
|
9.73
|
1(2.2%)
|
|
Total
|
94(100%)
|
63.38
|
11.99
|
6(6.4%)
|
There is no significant association between the BMI & the incidence of DVT at (p > 0.05). The incidence of DVT was slightly higher in the patients undergoing unilateral arthroplasty on the left side (p=0.864).
Risk factors and incidence of DVT
There was no significant association between the presence of CVS comorbid, previous respiratory illness, alcohol consumption, smoking, diabetes mellitus, hypertension and varicose veins with incidence of DVT (Table 2).
Table 2: Risk factors and incidence of deep vein thrombosis.
|
|
No. of patients
|
DVT positive
|
p value
|
|
CVS - Comorbid condition
|
|
|
Present
|
15(16%)
|
1(6.67%)
|
p=0.905
|
|
|
Absent
|
79(84%)
|
5(6.33%)
|
|
|
Total
|
94(100%)
|
6(6.4%)
|
|
Respiratory - Comorbid condition
|
|
|
Present
|
11(11.7%)
|
2(18.18%)
|
p=0.60
|
|
|
Absent
|
83(88.3%)
|
4(4.81%)
|
|
|
Total
|
94(100%)
|
6
|
|
Alcohol
|
|
|
Present
|
22(23.4%)
|
1(4.5%)
|
p=0.687
|
|
|
Absent
|
72(76.6%)
|
5(6.9%)
|
|
|
Total
|
94(100%)
|
6(6.4%)
|
|
|
|
|
|
|
|
Smoking
|
|
|
Present
|
29(30.9%)
|
1(3.4%)
|
p=0.437
|
|
|
Absent
|
65(69.1%)
|
5(7.7%)
|
|
|
Total
|
94(100%)
|
6
|
|
Diabetes mellitus
|
|
|
Present
|
37(39.4%)
|
4(10.8%)
|
p=0.157
|
|
|
Absent
|
57(60.6%)
|
2(3.5%)
|
|
|
Total
|
94(100%)
|
6(6.4%)
|
|
Hypertension
|
|
|
Present
|
43(45.7%)
|
1(2.3%)
|
p=0.14
|
|
|
Absent
|
51(54.3%)
|
5(9.8%)
|
|
|
Total
|
94(100%)
|
6(6.4%)
|
|
Varicose veins
|
|
|
Present
|
14(14.9%)
|
1(7.1%)
|
p=0.9
|
|
|
Absent
|
80(85.1%)
|
5(6.3%)
|
|
|
Total
|
94(100%)
|
6
|
Surgical factors and incidence of DVT
Patients who underwent cemented hemiarthroplasty showed a significant increase in the incidence of DVT (Table 3). There is no significant association between type of anesthesia & the incidence of DVT at (p > 0.05). The incidence of DVT in the patients who underwent total knee replacement and for whom tourniquet was applied was 3.6% which was not found to be significant. There was no significant difference seen in the mean duration of surgery, blood loss and units of blood transfused between the group which developed DVT and the group which did not develop DVT. There is no significant association between blood group & the incidence of DVT at (p > 0.05).
Table 3: Type of surgery and incidence of deep vein thrombosis.
|
Sugery
(No. of patients)
|
Cemented/ Uncemented
|
Incidence
of DVT
|
p value
|
|
THR (23)
|
Cemented, 11(47.8%)
|
0(0%)
|
p=0.328
|
|
Uncemented, 12(52.2%)
|
1(8.3%)
|
|
HEMI (25)
|
Cemented, 8(32%)
|
3(37.5%)
|
p=0.044*
|
|
Uncemented, 17(68%)
|
1(5.9%)
|
|
TKR (46)
|
Cemented, 46
|
1(2.2%)
|
|
|
Total
|
94
|
6(6.4%)
|
*(p<0.05)
Mean preoperative immobility period and mean postoperative immobility period were increased in the group of patients which developed DVT but the difference was not significant when compared to the group which did not develop DVT (Table 4).
Table 4: Period of immobility and incidence of deep vein thrombosis (DVT).
|
|
|
No. of patients
|
Mean
(Days)
|
Std. Dev.
|
|
Preoperative immobility
|
|
|
DVT + Group
|
6
|
5
|
6.39
|
|
|
DVT- Group
|
88
|
2.14
|
6.4
|
|
Postoperative ambulation
|
|
|
DVT + Group
|
6
|
9.83
|
10.94
|
|
|
DVT- Group
|
88
|
6.93
|
7.31
|
Clinical features and incidence of DVT
In this study 6 patients developed symptomatic DVT. All were diagnosed and confirmed by color doppler (Figure 1).
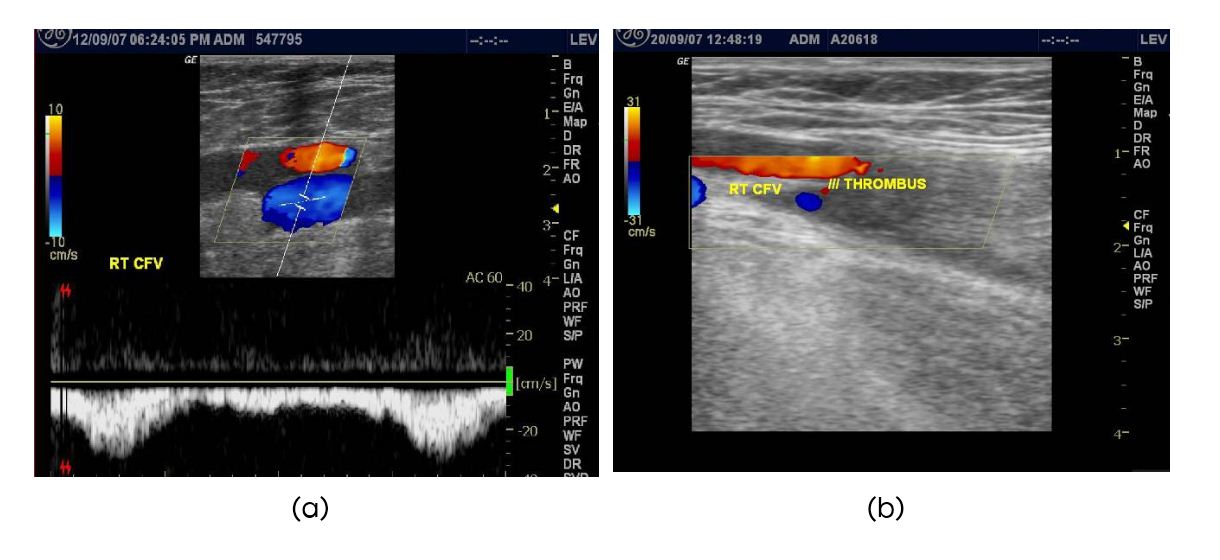
Figure 1: Color doppler (a) Preoperative doppler, (b) Early post-operative doppler showing thrombus in the right CFV.
Three patients developed DVT in the early postoperative period (4-13 days). Three patients developed DVT in the late postoperative period (28-42 days). Average time of presentation of DVT was 19.67 days. One patient in our study sample (1.06%) developed non-fatal pulmonary embolism after late onset DVT on the 35th day.
Early clinical features of DVT were analyzed for all the 94 patients but late clinical features of DVT were analyzed for 91 patients only as the 3 patients who had developed early DVT and were on treatment for the same were not included in the analysis of the late onset clinical features. Significant association was noted in this study between calf muscle tenderness and positive Homan’s sign in patients who developed early DVT. Leg pain, swelling (Figure 2), calf muscle tenderness and Homans’ sign were significant clinical features in patients who developed late DVT.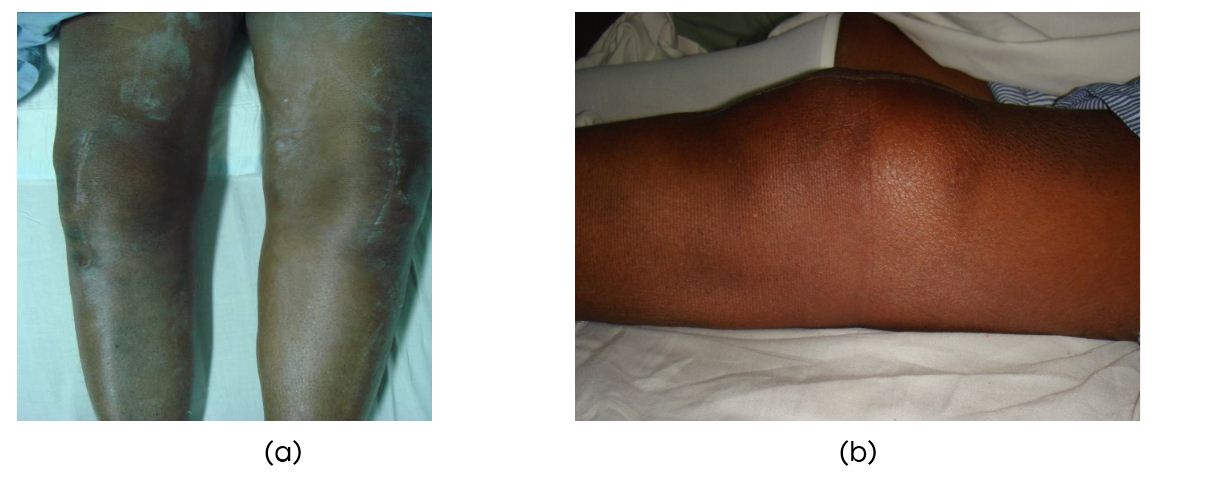
Figure 2a,b: Swelling noted in the left leg in a patient who underwent bilateral total knee replacement and was diagnosed positive for deep vein thrombosis.
Side and site of DVT
Deep vein thrombosis was more common in the operated leg. Proximal DVT was more common.
Prophylaxis and incidence of DVT
All the patients in our study were educated about the risk of DVT and were taught ankle mobilization exercises and to maintain adequate hydration during the post-operative period. All the patients who received chemical thromboprophylaxis were given the same for approximately 10 days. In our study 56.4% of the patients were thromboprophylaxed and the incidence of DVT amongst them was 3.8%. 43.6% of the patients were not thromboprophylaxed and the incidence of DVT amongst them was 9.8 (Tables 5 & 6).
Table 5: Patients on chemoprophylaxis and incidence of deep vein thrombosis.
|
LMWH
|
No. of patients
|
DVT positive
|
% (Within LMWH)
|
p value
|
|
Yes
|
53(56.4%)
|
2
|
3.8
|
p= 0.239
|
|
No
|
41(43.6%)
|
4
|
9.8
|
|
Total
|
94 (100%)
|
6
|
|
Abbreviations: LMWH : Low molecular weight heparin
Table 6: Surgery wise patients on chemoprophylaxis and incidence of deep vein thrombosis.
|
Surgery (No. of patients)
|
LMWH
(Low molecular weight heparin)
|
Incidence of DVT
|
p value
|
|
THR (23)
|
Thromboprophylaxed, 14(60.9%)
|
1(7.1%)
|
p=0.412
|
|
Not thromboprophylaxed, 9(39.1%)
|
0(0%)
|
|
HEMI (25)
|
Thromboprophylaxed, 13(52%)
|
0(0%)
|
p=0.023*
|
|
Not thromboprophylaxed, 12(48%)
|
4(33.33%)
|
|
TKR (46)
|
Thromboprophylaxed, 26(56.5%)
|
1(3.9%)
|
p=0.375
|
|
Not thromboprophylaxed, 20(43.5%)
|
0(0%)
|
|
TOTAL
|
94
|
6(6.4%)
|
|
Abbreviations: LMWH: Low molecular weight heparin; *p<0.05
Discussion
In most of the studies on the incidence of deep vein thromboembolic disease, the incidence is said to be high in the western countries. There is a deep- rooted belief among clinicians that DVT is rare in Asians. There have been reports that cite a prevalence of 2.6% to 17% amongst Chinese population and similar prevalence among Malaysians and Thai patients [1]. There are other studies from Asia which have shown a varying degree of incidence of DVT.
In the study by Dhillon et al. [2], the incidence of DVT in patients who underwent surgery for fracture of proximal femur or for total hip replacement or total knee replacement was 62.5% (total knee replacement: 76.5%, total hip replacement: 64.3%, fracture group: 50%). Prospective multicentric study by Rajagopalan N [3] showed an incidence of 7.8% in the Indian population. A prospective study by Agarwala S et al. [4] showed that the incidence of DVT in Indians was 52.1%. The incidence of DVT after total hip arthroplasty and total knee arthroplasty were 9.1% and 4.1% respectively in a study done in the Japanese population [5].
All the above-mentioned studies focus our attention to the fact that incidence of DVT is raised in different studies among the Asian groups. Hence, we designed a study in order to find out the incidence of DVT in patients undergoing major lower limb orthopaedic surgeries like hip and knee arthroplasty. The incidence of DVT in our study is 6.4%.
In our study, DVT was observed in patients of all age groups with an increasing incidence of DVT with advancing age. 83.3% of the patients positive for DVT were above 60 years. The mean age of the patients in the study was 63 years (Min-36 years and max-84 years). In the study by Bjørnarå BT et al. [6] the mean age of patients who developed venous thromboembolism was 69 and 73 years in THR and TKR respectively.
We observed DVT to be common in patients who underwent hip arthroplasty with a significant incidence (p<0.05) in the patients who underwent hemiarthroplasty. This could be due to the increased mean age of the patients undergoing hemiarthroplasty. There was no significant association noted in our study between bilateral total knee replacement and the incidence of DVT.
Our study showed an increased incidence of DVT in females similar to the study by Bjornara BT et al. [6] while the study by Rajagopalan N et al. [3] showed an increased incidence in males. Coon WW [7] in his study has found that the incidence of DVT is one and half times more common in obese patients. We observed an increased incidence in patients who were overweight (BMI>25) but it was not statistically significant similar to the study by Andrew JG et al. [8].
We observed that 6.67% of the patients with previous CVS comorbid conditions, and 18.18% of the patients with previous respiratory comorbid conditions developed DVT, showing no significant statistical association (p>0.05). We observed that the incidence of DVT was 3.4 % amongst smokers and 4.5% in people who had history of consumption of alcohol. This was statistically not significant.
10.8% of the diabetics, 2.3% of the hypertensives and 7.1% of the patients with varicose veins developed DVT and these were not significant risk factors in our study. This observation was similar to the study by Rajagopalan N [3]. Comorbid conditions like previous major surgeries, paralysis due to stroke, chemotherapy for malignancy, chronic kidney disease though theoretically are associated with higher incidence of DVT, were not significant risk factors in this study.
Incidence of DVT based on surgical procedures in our study was THR-4.3%, hemiarthroplasty-16%, and TKR- 2.2%. One patient in our study sample (1.06%) developed non-fatal pulmonary embolism after late onset DVT. He had under gone hemiarthroplasty. Study by Agarwala S et al. [4] in Indians undergoing arthroplasty showed the incidence of DVT to be THR-42.9%, TKR-72.2% and overall 52.1%.
Francis et al. [9] found that the use of bone cement in THR increased the incidence of DVT. We observed, in this study, that there was a significant increase in incidence of DVT occurring in patients who underwent cemented hemiarthroplasty. Clarke MT et al. [10] concluded that the use of cement may affect the formation of DVT after joint replacement but does not appear to lead to an increased incidence.
As most of the patients in the study sample underwent surgery under spinal anesthesia + epidural anesthesia, (81 out of 94), it could not be compared with patients who underwent surgery under general anesthesia due to inadequate sample but in the study by Davis FM et al. [11] they concluded that spinal anesthesia reduces the risk of DVT in hip replacement surgeries
The incidence of DVT after total knee replacement performed under tourniquet has been reported to be between 72% [12] and 84% [13]. 46 patients underwent total knee replacement. Of them tourniquet was used in 28 patients (60.87%). The incidence of DVT in the patients for whom tourniquet was applied was 3.6% which was not found to be significant.
In this study there was no significant difference seen in the duration of surgery, blood loss and units of blood transfused in the group which developed DVT and the group which did not develop DVT and this is similar to the study by Rajagopalan N [3]. 50% of the study sample who developed DVT had a blood group B+. There was no significant association between blood group & the incidence of DVT at (p > 0.05).
In our study the patients who developed DVT had a mean pre-operative immobility period of 5±6.39 days while the patients who did not develop DVT had a mean pre-operative immobility period of 2.14±6.4 days but there was no significant difference noted between the two groups.
Studies have established that patients who were mobilized early in the post-operative period had lower incidence of DVT than patients who were mobilized late [14]. In our study the patients who developed DVT had a mean post-operative immobility period of 9.83±10.94 days while the patients who did not develop DVT had a mean post-operative immobility period of 6.93±7.31days but there was no significant difference noted between the two groups.
In our study 6 patients developed symptomatic DVT. All were diagnosed and confirmed by color doppler [15]. A study done by Nagi ON et al. [16] in North India analysed the patients using compression ultrasound technique and revealed an 8% incidence of proximal DVT after major orthopaedic procedures and found it as a good modality to pick up this complication. Three patients developed DVT in the early postoperative period (4-13 days), three patients developed DVT in the late postoperative period (28-42 days). Average time of presentation of DVT was 19.67 days. One patient amongst them developed non-fatal pulmonary embolism after late onset DVT on the 35th day. In the study by Dahl OE et al. [17] DVT appeared, on average 27 days after Total hip replacement and 17 days after total knee arthroplasty.
Significant association was noted in this study, between calf tenderness and positive Homans’ sign, in patients who developed early DVT while leg pain, leg swelling, calf tenderness and Homans’ sign were significant clinical features in patients who developed late DVT.
In our study, there were patients with clinical evidence of DVT but were negative for DVT on color doppler. Therefore there was a mismatch between the clinical findings and color doppler for DVT. In our study proximal DVT incidence (66.7%) was higher when compared to distal DVT similar to study by Rajagopalan N [3]. Study by Agarwala S et al. [4] showed that the incidence of distal thrombi was higher in Indian patients undergoing arthroplasty. The study by Kim YH et al. [18] showed that all the thrombi regardless of their site and size resolved spontaneously without associated pulmonary embolism.
We observed an increased incidence of DVT in the operated limb than in the contra lateral limb similar to study by Rajagopalan N [3]. DVT developed in the non-operated lower limb in approximately 16.7% of the patients in our study. Hence patients have to be screened for DVT irrespective of the clinical findings and at the same time both the lower limbs have to be screened for DVT. Martin A et al. [19] showed that there was a significant reduction in both venous capacitance and venous outflow affecting both legs but greater in the operated leg.
56.4% of the patients in our study population were given chemical thromboprophylaxis and amongst them the incidence of DVT was 3.8% while 46.3% who were not given chemical thromboprophylaxis had an incidence of 9.8% (p=0.239). Patients undergoing hemiarthroplasty who were not given chemical thromboprophylaxis showed a significant increase in incidence of DVT in our study (p=0.023). Study by Agarwala S [4] showed an incidence of 43.2% in the arthroplasty group which was given chemical thromboprophylaxis and 60% in the arthroplasty group which was not given chemical thromboprophylaxis and this was statistically significant.
All the patients in our study were educated about the risk of DVT and were taught ankle mobilization exercises and to maintain adequate hydration during the post-operative period. 66.7% of the patients who developed DVT did not receive any mechanical prophylaxis and 50% of the patients who developed DVT did not receive either chemical or mechanical prophylaxis (p=0.788) but we cannot compare the groups as the samples are not equal.
Conclusion
The incidence of deep vein thrombosis (DVT) in this study is 6.4% amongst patients undergoing hip and knee arthroplasty. Factors like increase in age, increased preoperative immobility due to hip fractures, bilateral knee surgeries, patients undergoing cemented hemiarthroplasty, increased postoperative immobility, and patients not given any form of prophylaxis showed increased incidence of DVT. Postoperative chemoprophylaxis for patients who underwent arthroplasty showed a reduction in the incidence of DVT. All the comorbid conditions which were considered as risk factors were not significantly associated with increased incidence of DVT in this study. DVT can early or late postoperative period. DVT can occur even in the contra lateral limb. So both the lower limbs need to be screened. The study has it’s limitation that, it derives its conclusion from a single center and from a small volume of patients.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Nandi PL, Li WS, Leung R, Chan J, Chan HT. Deep vein thrombosis and pulmonary embolism in the Chinese population HKMJ. 1998; 4:305–310.
[2] Dillon KS, Askander A, Doraisamy S. Postoperative deep vein thrombosis in Asian patients is not a rarity: A prospective study of 88 patients with no prophylaxis. J Bone Joint Surg Br. 1996; 78(3):427–429.
[3] Rajagopalan N. Thromboprophylaxis by Dalteparin sodium in elective major orthopaedic surgery - A multicentric Indian study. Indian J Orthop. 2003; 37(2):4.
[4] Agarwala S, Bhagwat A, Modhe J, Dastur F D, Patil S. Incidence of deep vein thrombosis in Indian patients: A prospective study in 104 patients. Indian J Orthop. 2003; 37(2):5.
[5] Sudo A, Sano T, Horikawa K, Yamakawa T, Shi D, et al. The incidence of deep vein thrombosis after hip and knee arthroplasties in Japanese patients: A prospective study. J Orthop Surg. 2003; 11(2):174–177.
[6] Bjørnarå BT, Gudmundsen TE, Dahl OE. Dahl Frequency and timing of clinical venous thromboembolism after major joint surgery. J Bone Joint Surg Br. 2006; 88(3): 386–91.
[7] Coon WW. Epidemiology of venous thromboembolism. Ann Surg. 1977; 186(2):149–164.
[8] Andrew JG, Palan J, Kurup HV, Gibson P, Murray DW, et al Obesity in total hip replacement. J Bone Joint Surg Br. 2008; 90(4):424–429.
[9] Francis CW, Marder VJ, Evarts CM. Lower risk of thromboembolic disease after total hip replacement with non-cemented than with cemented prostheses. Lancet. 1986;1:769–71.
[10] Clarke MT, Green JS, Harper WM, Gregg PJ. Cement as a risk factor for deep vein thrombosis: Comparison of cemented TKR, uncemented TKR and cemented THR. J Bone Joint Surg Br. 1998; 80(4):611–613.
[11] Davis FM, Laurenson VG, Gillespie WJ, Wells JE, Foate J, et al. Deep vein thrombosis after total hip replacement. A comparison between spinal and general anaesthesia. J Bone Joint Surg Br. 1989; 71(2):181–185.
[12] Lotke P A, Faralli V J, Orenstein E M, Ecker M L. Blood loss after total knee replacement: effects of tourniquet release and continuous passive motion. J Bone Joint Surg (Am) 1991; 73: 1037-40.
[13] Stulberg BN, Insall JN, Williams GW, Ghelman B. Deep-vein thrombosis following total knee replacement. An analysis of six hundred and thirty-eight arthroplasties. J Bone Joint Surg Am. 1984; 66(2):194–201.
[14] Pearse EO, Caldwell BF, Lockwood RJ, Hollard J. Early mobilisation after conventional knee replacement may reduce the risk of postoperative venous thromboembolism. J Bone Joint Surg Br. 2007; 89(3):316–322.
[15] Grady-Benson JC, Oishi CS, Hanson PB, Colwell CW Jr, Otis SM, et al. Postoperative surveillance for deep venous thrombosis with duplex ultrasonography after total knee arthroplasty. J Bone Joint Surg Am. 1994; 76(11):1649–1657.
[16] Nagi ON, Dhillon MS, Katariya S, Mujeeb MdS . Deep vein thrombosis after major surgery - Evaluation by compression ultrasonography. Indian J Orthop. 1999; 33(3):200–203.
[17] Dahl OE, Gudmundsen TE, Haukeland L. Late occurring clinical deep vein thrombosis in joint operated patients. Acta Orthop Scand. 2000; 71(1):47–50.
[18] Kim YH, Kim JS. Incidence and natural history of deep-vein thrombosis after total knee arthroplasty: A Prospective, Randomized study. J Bone Joint Surg Br. 2002; 84(4):566–70.
[19] Mcnally MA, Mollan RA. Total hip replacement, lower limb blood flow and venous thrombogenesis. J Bone Joint Surg Br. 1993; 75(4):640–644.