Full Text
Introduction
Pemphigus vulgaris is an uncommon chronic disease [1]. It represents a group of autoimmune diseases of unknown etiology. It is characterized by the development of IgG antibodies against the desmogleins present in keratinocytes. This causes acantholysis [2]. Two clinical subtypes have been reported, mucosal form and mucocutaneous form. The mean age of presentation is 40-50 years. According to Espana et al. females are more commonly involved than males [3]. Wohl and Brenner, in their study found a correlation between pemphigus and ultraviolet radiation and pesticides [4].
The oral mucosa is the most common location of pemphigus lesions. Erosions may extend to the pharynx, larynx, esophagus, and respiratory system [6]. Pemphigus with primary laryngeal involvement is extremely rare [5]. The frequency with which it occurs is unknown. The diagnosis of laryngeal pemphigus is based on proper clinical examination, endoscopic laryngeal evaluation, biopsy, immunohistochemistry and immunofluorescence.
In the present paper, we are describing a rare case of pemphigus vulgaris with primary laryngeal involvement. Patient presented with stridor to emergency department. Patient doesn’t have any other mucosal or cutaneous lesions.
Case report
A 57-year-old male diabetic patient presented with difficulty in breathing and change of voice. He was a smoker and alcoholic. He also had throat pain, dysphagia and fever. As the patient was in stridor, emergency tracheostomy was done, Followed by direct laryngoscopy and biopsy. Patient was given initial supportive measures like rehydration, stabilising the vitals in the ER. Direct laryngoscopy showed smooth mucosa covered growth in right pyriform sinus, with pooling of saliva. Right vocal cord was fixed (Figure 1).
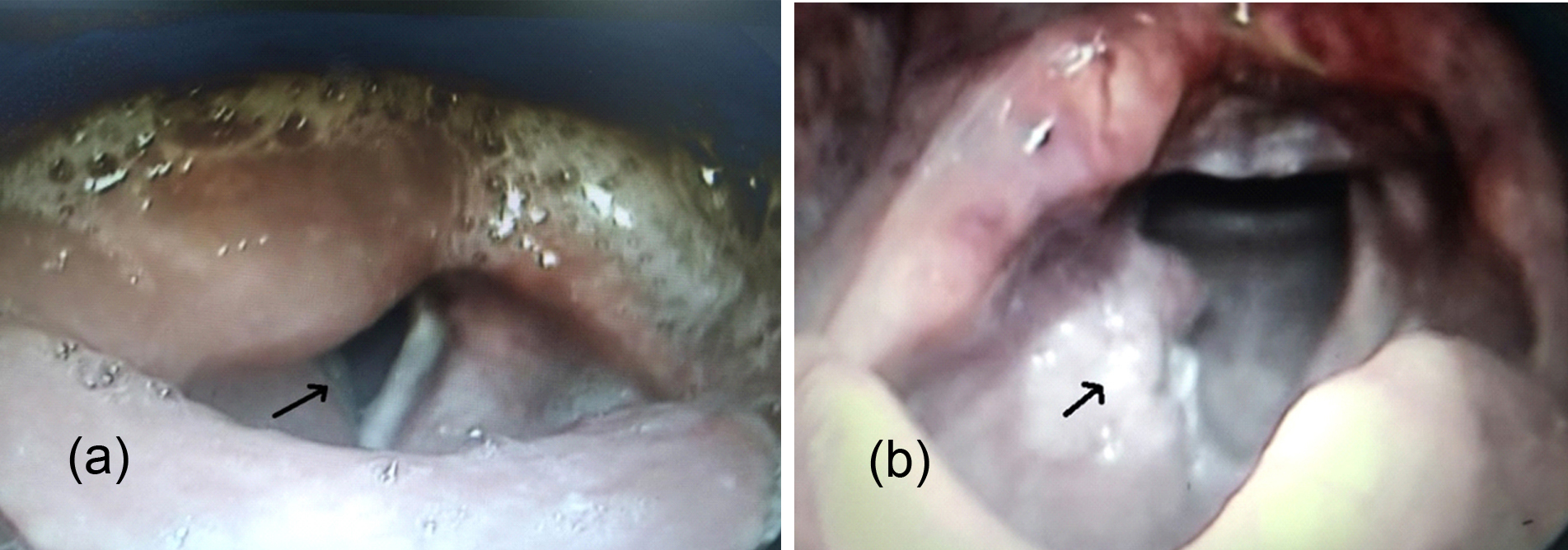
Figure 1a,b: Laryngoscopy findings; pooling of saliva, growth in pyriform sinus, fixed vocal cord.
Biopsy was taken from the growth and sent for histopathological examination. CT scan of the neck was done (Figure 2) in axial, coronal and sagittal planes, showed large heterogeneously enhancing mass lesion in right pyriform fossa measuring 2.5×3.5×4 (5cms). Better delineation of the mass was seen in these films shown.
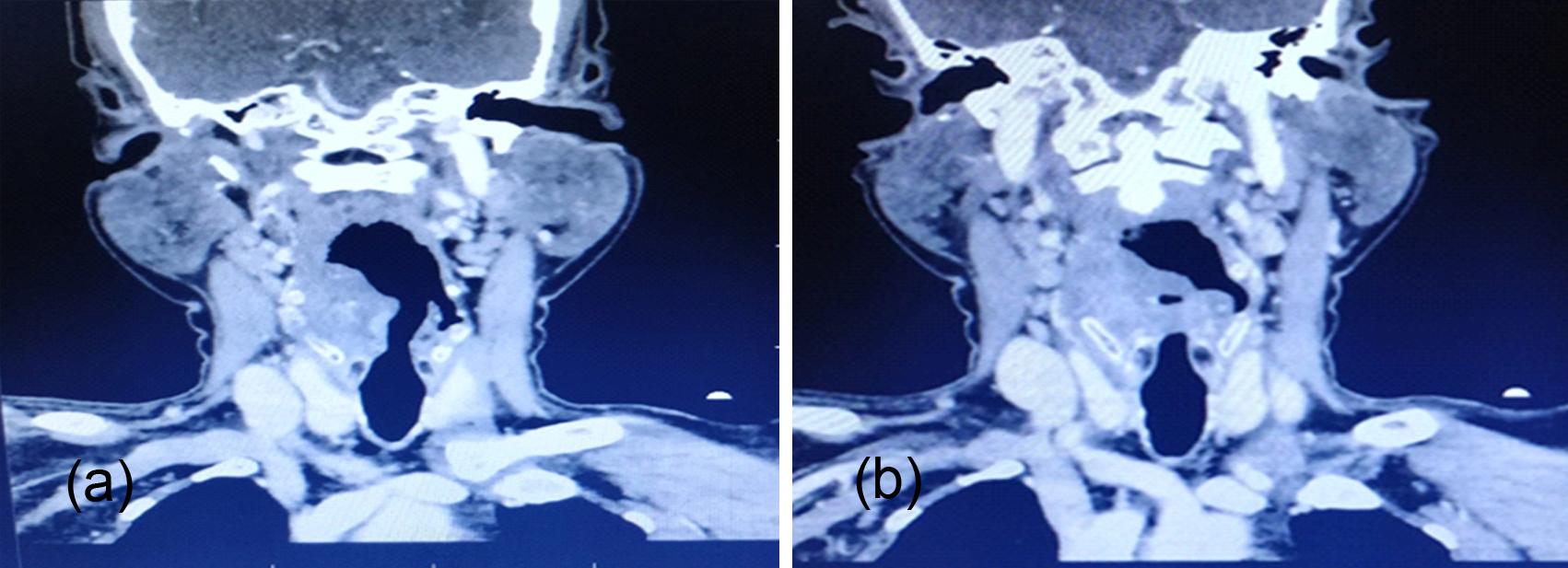
Figure 2: CT- mass in pyriform fossa.
Doppler study of showed the mass lesion close to right carotid artery. Patient was anemic, erythrocyte sedimentation rate (ESR) was high (75mm/hr). Monteux test was positive. Diagnostic possibilities of laryngeal malignancy, Koch’s were thought of. But to our surprise the histopathological examination was reported as acantholytic lesions suggestive of pemphigus (Figure 3).

Figure 3a,b: Intra epithelial bulla with acantholysis. Basal lamella is preserved.
The diagnosis was confirmed with immunofluorescence study. Even though the patient doesn’t have any cutaneous lesions, but on the advice of dermatologist biopsy from buccal mucosa was taken. It was reported as acanthosis and acantholysis suggestive of pemphigus. Patient was counselled and put on high dose of oral steroids and was followed up regularly. Laryngoscopies were done periodically, showed gradual decrease in the size of lesion. patient became hemodynamically stable. Tracheostomy was decannulated successfully (Figure 4).
Figure 4: Tracheostomy decannulated.
Discussion
Pemphigus vulgaris is an autoimmune bullous disease characterised by development of intraepithelial blisters on skin or mucosa. This is secondary to IgG antibody against desmoglein present in keratinocytes. It may associate with other autoimmune disorders like Hashimoto’s, Sjogren’s, lupus etc.
Laryngeal pemphigus is a very rare disease with an estimated incidence of 0.7 patients per 1,00,000. The mean age of presentation is 40-50 years. Two clinical subtypes have been defined, mucosal and mucocutaneous form. Various types of pemphigus diseases include –P. vulgaris, P. Foliaceous, P. vegetans, P. erythematosus and P. herpetiformis.
Generally, the mucosal lesions precede the skin lesions. It is uncommon for the diagnosis to be made based on biopsy of oral mucosa.
There is currently no uniform classification of laryngeal pemphigus with regard to lesion characteristics and locations within supraglottis and glottis. Mohamoud et al. proposed a classification of grading of laryngeal lesions according to the site of involvement (Table 1) [7].
Table 1: Classification of grading of laryngeal lesions.
|
Grade
|
Site of involvement
|
|
1
|
Epiglottis
|
|
2
|
Supraglottis
|
|
3
|
Pyriform sinus
|
|
4
|
Ventricular folds or vocal folds
|
The supraglottic region is the most commonly involved, followed by glottis. Laryngeal involvement in pemphigus varies from hoarseness of voice to serious oedema leading to airway obstruction and emergency tracheostomy as happened in our case. However, the common findings are oedema, ulceration, bullae, membranes, and stenosis.
Endoscopic examination is important in patients both with and without laryngeal symptoms, in order to enable examination of a greater area of mucosa and to guide therapy. In the differential diagnosis of pemphigus, the two important clinical signs are Nikolsky sign and Asboe -Hansen sign.
Microbial infections of the skin lesions specially with S. aureus is a serious complication of pemphigus, and may cause septicaemia and death. The presence of lesions in the larynx requires the use of more aggressive therapy because of the risk of acute respiratory failure.
Corticosteroids especially high doses are the treatment of choice in pemphigus. They have reduced the morbidity and mortality. Corticosteroids in combination with immunosuppressive agents such as azathioprim, cyclophosphamide, ciclosporins are recommended for more serious cases. Plasmapheresis, dapsone, tetracyclines, niacinamide have also been used in the management. Refractory cases can be treated with IV administration of immunoglobulins, extracorporeal photopheresis. Prophylactic administration of antibiotics is important against staph infections.
Conclusion
Primary pemphigus involving larynx though rare must be considered in the differential diagnosis of obscure laryngeal lesions. Laryngeal findings must be considered at the beginning of diagnosis of pemphigus vulgaris. Patients with pemphigus need endoscopic laryngeal examination whether they have laryngeal symptoms or not. This is because laryngeal involvement warrants aggressive treatment to prevent life threatening complications. ENT surgeons should be aware of the pemphigus as primary laryngeal manifestation in order to investigate and manage patients accordingly.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Vasiliou A, Nikolopoulos TP, Manolopoulos L, Yiotakis J. Laryngeal pemphigus without skin manifestations and review of the literature. Eur Arch Otorhinolaryngol. 2007; 264(5):509–512.
[2] Bansal M. Is laryngeal involvement in pemphigus vulgaris rare? A review. Int J Res Dermatol. 2015; 1(1):3–6.
[3] Espana A, Fernandez S, del Olmo J, Marquina M, Pretel M, et al. Ear, nose and throat manifestations in pemphigus vulgaris. Br J Dermatol. 2007; 156(4):733–737.
[4] Wohl Y, Brenner S. Pemphigus in Israel- an epidemiologic analysis of cases in search of risk factors. Isr Med Assoc J. 2003; 5(6):410–412.
[5] Obregon G. Pemphigus of larynx. Ann Oto Rhino Laryngol. 1957; 66(3):649–655.
[6] Laskaris G. Stomatology – coloured Atlas, 2nd edn. Lista’s Medical Publications, Athens. 1998; pp.312–324.
[7] Mahmoud A, Miziara ID, Costa KC, Santi CG, Maruta CW, et al. Laryngeal involvement in pemphigus vulgaris: a proposed classification. J Laryngol Otol. 2012; 126:1041–1044.